Crohn’s disease is a chronic inflammatory bowel disease (IBD) that can affect any part of the gastrointestinal tract, from the mouth to the anus. It is characterized by periods of exacerbation and remission, leading to a range of symptoms including abdominal pain, diarrhea, weight loss, and fatigue. The exact cause of Crohn’s disease remains elusive, but it is believed to involve a combination of genetic predisposition, immune system dysfunction, and environmental factors.
The disease can manifest at any age, though it is most commonly diagnosed in young adults. The impact of Crohn’s disease extends beyond physical symptoms; it can significantly affect a patient’s quality of life. Individuals may experience social isolation due to the unpredictable nature of flare-ups, which can lead to anxiety and depression.
The chronic nature of the disease often necessitates long-term management strategies, including dietary modifications and medication adherence. Understanding Crohn’s disease is crucial for both patients and healthcare providers, as it lays the foundation for effective treatment and management strategies.
Key Takeaways
- Crohn’s disease is a chronic inflammatory condition affecting the digestive tract with complex treatment needs.
- Clinical trials are essential for evaluating the safety and effectiveness of new Crohn’s disease therapies.
- Current treatments include medications like anti-inflammatories, immunosuppressants, and biologics, but challenges remain.
- Recent clinical trials have introduced promising new therapies aiming to improve patient outcomes and reduce side effects.
- Patient participation is crucial for advancing research, though trials face challenges such as recruitment and variability in disease presentation.
Understanding Clinical Trials
Clinical trials are research studies that evaluate the safety and efficacy of new treatments or interventions in human participants. They are essential for advancing medical knowledge and improving patient care. In the context of Crohn’s disease, clinical trials play a pivotal role in testing new medications, therapies, and treatment protocols.
These trials are typically conducted in phases, starting with small groups of participants to assess safety before expanding to larger populations to evaluate effectiveness. The design of clinical trials can vary significantly. Some trials may focus on comparing a new drug to a placebo, while others might compare two active treatments.
Randomized controlled trials (RCTs) are considered the gold standard in clinical research because they minimize bias and provide robust data on treatment outcomes. Participants in clinical trials often receive close monitoring and care from healthcare professionals, which can be an added benefit for those living with chronic conditions like Crohn’s disease.
Current Treatment Options for Crohn’s Disease
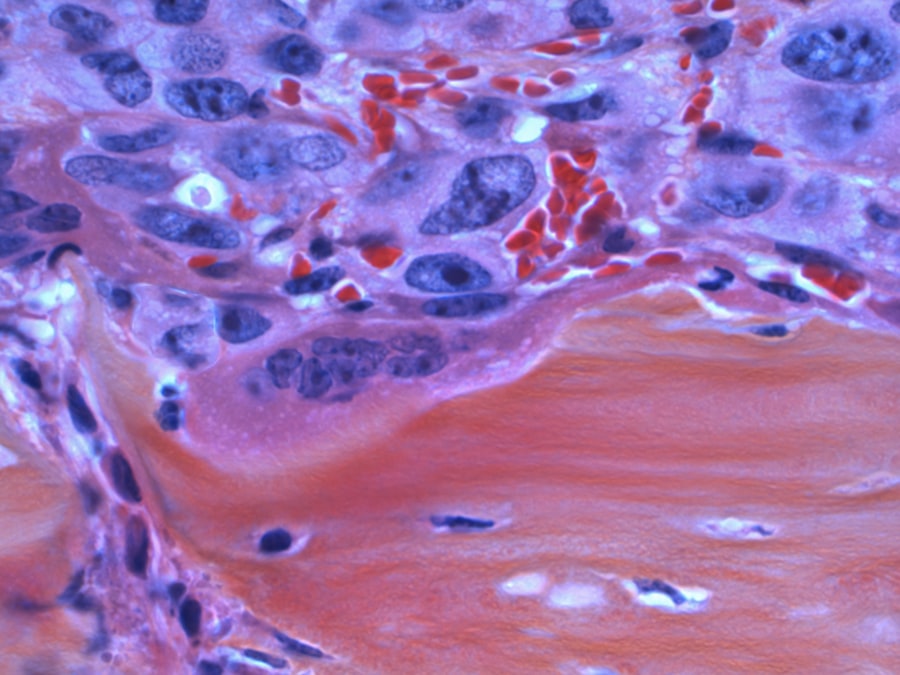
The management of Crohn’s disease typically involves a combination of medication, lifestyle changes, and sometimes surgical interventions. Current treatment options include anti-inflammatory drugs such as corticosteroids, immunosuppressants like azathioprine and methotrexate, and biologics that target specific pathways in the immune response. Biologics, such as infliximab and adalimumab, have revolutionized the treatment landscape for Crohn’s disease by providing targeted therapy that can induce and maintain remission in many patients.
In addition to pharmacological treatments, dietary management plays a crucial role in managing symptoms. Some patients find relief through specific diets that eliminate trigger foods or focus on nutrient-dense options. Nutritional support may also be necessary for those experiencing malnutrition due to the disease’s impact on absorption.
Surgical options are considered when medical management fails or complications arise, such as strictures or fistulas. Resection of affected bowel segments can provide relief but does not cure the disease, as Crohn’s can recur in other areas of the gastrointestinal tract.
Advancements in Crohn’s Disease Clinical Trials
Recent years have seen significant advancements in clinical trials related to Crohn’s disease, particularly with the introduction of novel therapies and improved trial designs. Researchers are increasingly utilizing biomarkers to identify patients who are more likely to respond to specific treatments, thereby personalizing therapy and enhancing outcomes. This approach not only improves patient care but also streamlines the drug development process by focusing on the most promising candidates.
Moreover, advancements in technology have facilitated remote monitoring and telemedicine in clinical trials. Patients can participate from their homes while still receiving comprehensive care and support from trial coordinators. This flexibility has been particularly beneficial during the COVID-19 pandemic, allowing ongoing research without compromising patient safety.
Additionally, adaptive trial designs enable researchers to modify protocols based on interim results, potentially accelerating the development of effective therapies for Crohn’s disease.
Promising New Therapies and Treatments
| Trial Phase | Number of Trials | Primary Outcome Measures | Average Duration (Months) | Common Interventions |
|---|---|---|---|---|
| Phase 1 | 15 | Safety and Tolerability | 6 | New Biologic Agents, Small Molecules |
| Phase 2 | 30 | Efficacy and Dose Ranging | 12 | Immunomodulators, Biologics |
| Phase 3 | 20 | Clinical Remission Rates, Mucosal Healing | 18 | Biologics, Combination Therapies |
| Phase 4 | 10 | Long-term Safety and Effectiveness | 24 | Approved Drugs Post-Marketing |
The landscape of Crohn’s disease treatment is evolving rapidly with the emergence of promising new therapies. One area of focus is small molecules that target specific pathways involved in inflammation and immune response. For instance, Janus kinase (JAK) inhibitors have shown potential in clinical trials for their ability to modulate immune signaling pathways effectively.
These oral medications offer an alternative to traditional biologics and may provide more convenient options for patients. Another exciting development is the exploration of microbiome-based therapies. Research has indicated that gut microbiota play a significant role in IBD pathogenesis, leading scientists to investigate fecal microbiota transplantation (FMT) as a potential treatment option.
Early studies suggest that FMT may help restore a healthy balance of gut bacteria in patients with Crohn’s disease, potentially reducing inflammation and improving symptoms. As research continues to unfold in this area, microbiome-targeted therapies could become a cornerstone of Crohn’s disease management.
Patient Participation in Clinical Trials
Patient participation is vital for the success of clinical trials, as it provides researchers with essential data on treatment efficacy and safety. Engaging patients in the research process not only enhances the quality of data collected but also empowers individuals to take an active role in their healthcare journey. Many patients with Crohn’s disease may be motivated to participate in clinical trials due to the desire for new treatment options or the hope of contributing to advancements in medical knowledge.
However, barriers to participation exist, including concerns about potential side effects, time commitments, and travel requirements for trial visits. To address these challenges, researchers are increasingly implementing strategies to improve patient recruitment and retention. This includes providing clear information about trial protocols, potential benefits, and risks involved.
Additionally, incorporating flexible scheduling and remote monitoring options can make participation more accessible for patients who may have difficulty attending in-person visits.
Challenges and Limitations in Crohn’s Disease Clinical Trials
Despite the advancements in clinical trials for Crohn’s disease, several challenges persist that can hinder research progress. One significant limitation is the heterogeneity of the disease itself; Crohn’s can present differently among individuals, making it difficult to establish standardized endpoints for treatment efficacy. This variability can complicate trial design and interpretation of results.
Furthermore, recruitment for clinical trials can be challenging due to strict eligibility criteria that may exclude many potential participants. This can lead to delays in trial initiation and completion, ultimately slowing down the development of new therapies. Additionally, funding constraints often limit the scope and scale of clinical trials, impacting the ability to explore innovative treatment options comprehensively.
Future Directions in Crohn’s Disease Research
Looking ahead, future directions in Crohn’s disease research are likely to focus on personalized medicine approaches that consider individual patient characteristics when developing treatment plans. The integration of genomics and proteomics into clinical practice may enable healthcare providers to tailor therapies based on a patient’s unique biological profile. Moreover, ongoing research into the gut microbiome holds promise for uncovering new therapeutic targets and strategies for managing Crohn’s disease.
As our understanding of the complex interactions between gut bacteria and host immune responses deepens, novel microbiome-based interventions may emerge as effective treatments. Finally, fostering collaboration between researchers, clinicians, patients, and advocacy groups will be essential for driving innovation in Crohn’s disease research. By working together, stakeholders can ensure that research efforts align with patient needs and priorities while advancing our understanding of this complex condition.
The future holds great potential for improving outcomes for individuals living with Crohn’s disease through continued research and innovation in treatment strategies.




