Melanoma, a malignant tumor of melanocytes, is one of the most aggressive forms of skin cancer. It arises from the pigment-producing cells in the skin and can occur anywhere on the body, although it is most commonly found on areas that have been exposed to the sun. The incidence of melanoma has been rising steadily over the past few decades, making it a significant public health concern.
According to the American Cancer Society, an estimated 99,780 new cases of melanoma will be diagnosed in the United States in 2022 alone, with approximately 7,650 deaths attributed to this disease. The increasing prevalence is often linked to factors such as excessive ultraviolet (UV) radiation exposure, particularly from tanning beds and sunbathing, as well as genetic predispositions. The prognosis for melanoma can vary significantly based on several factors, including the stage at which it is diagnosed.
Early-stage melanoma, when detected and treated promptly, has a high cure rate. However, once it metastasizes to other parts of the body, the survival rates drop dramatically. This stark contrast in outcomes underscores the importance of early detection and innovative treatment strategies.
As research continues to evolve, clinical trials play a crucial role in developing new therapies aimed at improving survival rates and quality of life for patients diagnosed with melanoma.
Key Takeaways
- Melanoma is a serious form of skin cancer with ongoing research focused on improving treatment outcomes.
- Clinical trials are essential for testing new melanoma therapies and advancing medical knowledge.
- Targeted therapies and immunotherapies are key treatment approaches being evaluated in melanoma clinical trials.
- Combination therapies and personalized medicine are emerging strategies to enhance treatment effectiveness.
- Future directions in melanoma research emphasize innovative treatments and tailored patient care.
Understanding Clinical Trials
Clinical trials are systematic investigations designed to evaluate the safety and efficacy of new medical interventions, including drugs, devices, or treatment protocols. These trials are essential for advancing medical knowledge and improving patient care. They typically progress through several phases: Phase I trials focus on safety and dosage; Phase II trials assess efficacy and side effects; and Phase III trials compare the new treatment against standard therapies in larger populations.
Each phase is meticulously designed to gather data that can inform future treatment options and guidelines. In the context of melanoma, clinical trials are particularly vital due to the disease’s complex nature and its ability to develop resistance to conventional therapies. Patients participating in these trials may gain access to cutting-edge treatments that are not yet available to the general public.
Moreover, clinical trials often provide a structured environment for monitoring patient responses and side effects, contributing valuable information that can lead to improved therapeutic strategies. The ethical considerations surrounding clinical trials are paramount; informed consent is required from all participants, ensuring they understand the potential risks and benefits involved.
Targeted Therapies in Melanoma Clinical Trials
Targeted therapies represent a significant advancement in the treatment of melanoma, particularly for patients with specific genetic mutations. One of the most notable examples is the use of BRAF inhibitors, which target mutations in the BRAF gene that are present in approximately 40-60% of melanoma cases. Drugs such as vemurafenib and dabrafenib have shown remarkable efficacy in shrinking tumors in patients with BRAF V600E mutations.
Clinical trials have demonstrated that these targeted therapies can lead to significant improvements in progression-free survival compared to traditional chemotherapy. In addition to BRAF inhibitors, MEK inhibitors like trametinib have been developed to target downstream signaling pathways involved in melanoma cell proliferation. Clinical trials combining BRAF and MEK inhibitors have shown enhanced efficacy and reduced resistance compared to monotherapy.
For instance, studies have indicated that the combination therapy can lead to higher response rates and longer-lasting effects than either drug alone. This approach exemplifies how targeted therapies can be tailored to individual patients based on their tumor genetics, offering a more personalized treatment strategy.
Immunotherapy in Melanoma Clinical Trials
Immunotherapy has revolutionized the treatment landscape for melanoma, harnessing the body’s immune system to fight cancer cells. Checkpoint inhibitors, such as pembrolizumab and nivolumab, have emerged as powerful tools in this domain. These agents work by blocking proteins that inhibit immune responses, thereby enhancing the ability of T-cells to recognize and attack melanoma cells.
Clinical trials have shown that these therapies can lead to durable responses in a subset of patients, even those with advanced disease. The success of immunotherapy has prompted extensive research into combination strategies that may further improve outcomes. For example, clinical trials are exploring the synergistic effects of combining checkpoint inhibitors with other modalities such as targeted therapies or radiation therapy.
The rationale behind these combinations lies in their potential to overcome resistance mechanisms that tumors may develop against single-agent therapies. Early results from these trials indicate promising response rates and improved survival outcomes, highlighting the need for continued exploration in this area.
Combination Therapies in Melanoma Clinical Trials
| Trial Name | Phase | Number of Participants | Intervention | Primary Outcome | Status |
|---|---|---|---|---|---|
| CheckMate 067 | Phase 3 | 945 | Nivolumab + Ipilimumab | Overall Survival at 5 years | Completed |
| KEYNOTE-006 | Phase 3 | 834 | Pembrolizumab vs Ipilimumab | Progression-Free Survival | Completed |
| IMspire150 | Phase 3 | 514 | Atezolizumab + Vemurafenib + Cobimetinib | Progression-Free Survival | Completed |
| RELATIVITY-047 | Phase 2/3 | 714 | Relatlimab + Nivolumab | Progression-Free Survival | Completed |
| COMBI-AD | Phase 3 | 870 | Dabrafenib + Trametinib | Relapse-Free Survival | Completed |
Combination therapies are increasingly recognized as a promising approach in melanoma treatment due to their potential to enhance efficacy while minimizing resistance. By targeting multiple pathways simultaneously, these strategies aim to improve patient outcomes significantly. For instance, combining immunotherapy with targeted therapy has gained traction in clinical trials.
Studies have shown that patients receiving both a BRAF inhibitor and a checkpoint inhibitor experience higher response rates than those receiving either treatment alone. Another area of exploration involves combining immunotherapy with traditional treatments such as chemotherapy or radiation therapy. While chemotherapy has historically been less effective for melanoma compared to other cancers, recent studies suggest that it may enhance the effectiveness of immunotherapy by inducing immunogenic cell death or modulating the tumor microenvironment.
Clinical trials investigating these combinations are ongoing, with early results indicating potential benefits in terms of overall survival and progression-free survival.
Personalized Medicine in Melanoma Clinical Trials
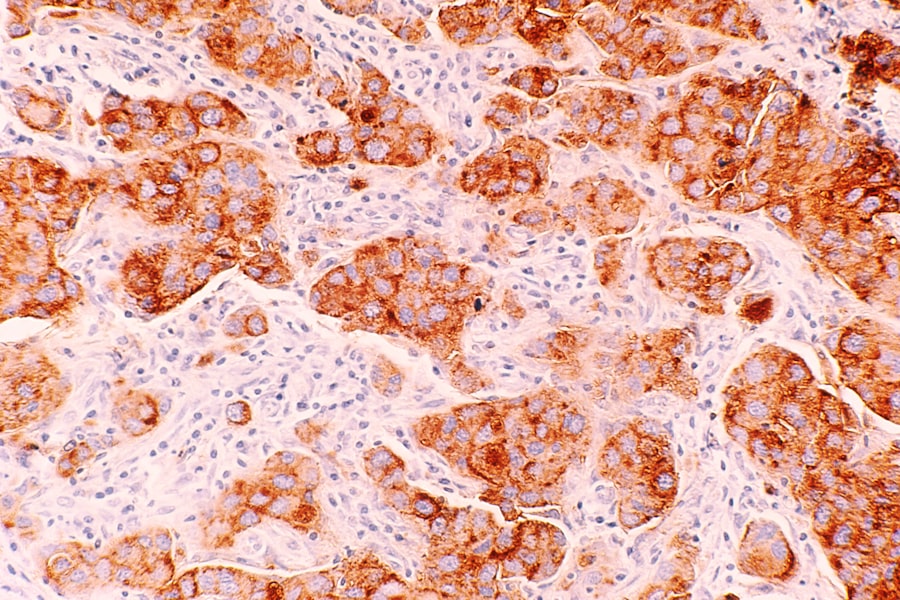
Personalized medicine represents a paradigm shift in oncology, focusing on tailoring treatment strategies based on individual patient characteristics, including genetic makeup and tumor biology. In melanoma, this approach is particularly relevant given the heterogeneity of the disease and its varied responses to treatment. Clinical trials are increasingly incorporating genomic profiling to identify specific mutations or biomarkers that can guide therapy selection.
For example, patients with tumors harboring specific mutations may benefit from targeted therapies designed for those alterations. Additionally, biomarkers such as PD-L1 expression levels can help predict responses to immunotherapy, allowing clinicians to select patients who are more likely to benefit from these treatments. The integration of personalized medicine into clinical trials not only enhances treatment efficacy but also minimizes unnecessary exposure to ineffective therapies.
Emerging Trends in Melanoma Clinical Trials
As research continues to advance, several emerging trends are shaping the future of melanoma clinical trials. One notable trend is the increasing use of real-world evidence (RWE) alongside traditional clinical trial data. RWE can provide insights into how treatments perform outside controlled trial settings, offering a more comprehensive understanding of their effectiveness and safety in diverse patient populations.
Another trend is the exploration of novel therapeutic agents beyond traditional small molecules and monoclonal antibodies. For instance, oncolytic viruses—viruses engineered to selectively infect and kill cancer cells—are being investigated in clinical trials for their potential to elicit robust anti-tumor immune responses. Additionally, adoptive cell transfer therapies, such as CAR T-cell therapy, are being explored for their ability to enhance immune responses against melanoma.
Furthermore, there is a growing emphasis on patient-reported outcomes (PROs) in clinical trials. Understanding how treatments impact patients’ quality of life is becoming increasingly important as survival rates improve. Incorporating PROs into trial designs allows researchers to capture valuable data on treatment tolerability and overall patient well-being.
Conclusion and Future Directions
The landscape of melanoma treatment is rapidly evolving due to ongoing research and innovation in clinical trials. As our understanding of the disease deepens, new therapeutic strategies continue to emerge, offering hope for improved outcomes for patients diagnosed with melanoma. The integration of targeted therapies, immunotherapies, combination approaches, and personalized medicine represents a multifaceted strategy that holds promise for addressing this challenging disease.
Looking ahead, future directions in melanoma clinical trials will likely focus on refining existing therapies while exploring novel agents and combinations that can further enhance efficacy and minimize resistance. The incorporation of real-world evidence and patient-reported outcomes will also play a crucial role in shaping treatment paradigms that prioritize not only survival but also quality of life for patients battling melanoma. As we continue to unravel the complexities of this disease through rigorous research efforts, there is optimism that we will achieve even greater strides in improving patient care and outcomes in melanoma management.