Ovarian cancer remains one of the most challenging malignancies to diagnose and treat, primarily due to its often asymptomatic nature in the early stages. As a result, many women are diagnosed at an advanced stage, which significantly complicates treatment options and outcomes. In response to this pressing health issue, numerous clinical trials have been initiated to explore new therapeutic avenues, improve existing treatment protocols, and enhance patient quality of life.
These trials are essential for advancing our understanding of ovarian cancer biology and for developing innovative strategies that can lead to better survival rates. Clinical trials in ovarian cancer encompass a wide range of research efforts, from testing novel drugs and combinations of therapies to evaluating the efficacy of existing treatments in different patient populations. The landscape of ovarian cancer research is continually evolving, driven by advancements in molecular biology, genetics, and technology.
As researchers delve deeper into the genetic underpinnings of ovarian cancer, they are uncovering potential biomarkers that could guide treatment decisions and improve patient outcomes. This article will explore various aspects of ovarian cancer trials, including targeted therapies, immunotherapy, early detection methods, and the role of genetic testing.
Key Takeaways
- Ovarian cancer trials are increasingly focusing on targeted therapies and personalized medicine to improve treatment efficacy.
- Immunotherapy is emerging as a promising approach in ovarian cancer treatment, with ongoing clinical trials exploring its potential.
- Advances in early detection and screening methods aim to identify ovarian cancer at more treatable stages.
- Genetic testing plays a crucial role in tailoring clinical trials and treatment plans for ovarian cancer patients.
- Patient advocacy and perspectives are integral to the design and success of ovarian cancer clinical trials.
Targeted Therapies and Personalized Medicine
Targeted therapies represent a paradigm shift in the treatment of ovarian cancer, moving away from traditional chemotherapy towards more precise interventions that focus on specific molecular targets associated with tumor growth and survival. These therapies aim to disrupt the signaling pathways that cancer cells rely on, thereby inhibiting their proliferation while sparing normal cells. One of the most notable examples is the use of PARP inhibitors, such as olaparib and niraparib, which have shown remarkable efficacy in patients with BRCA1 or BRCA2 mutations.
These drugs exploit the concept of synthetic lethality, where cancer cells deficient in DNA repair mechanisms are selectively killed when exposed to agents that further compromise their ability to repair DNA. Personalized medicine takes this concept a step further by tailoring treatment plans based on individual patient characteristics, including genetic makeup and tumor biology. For instance, genomic profiling of tumors can identify specific mutations or alterations that may predict responsiveness to certain targeted therapies.
This approach not only enhances the likelihood of treatment success but also minimizes unnecessary side effects associated with ineffective therapies. Ongoing clinical trials are investigating various combinations of targeted agents and their potential synergistic effects, aiming to optimize treatment regimens for different subtypes of ovarian cancer.
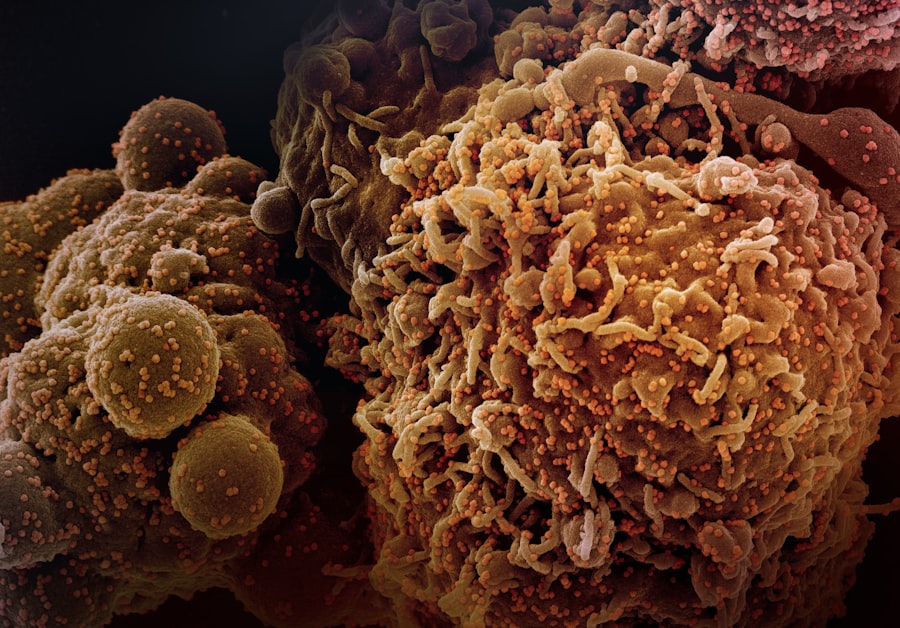
Immunotherapy and Ovarian Cancer
Immunotherapy has emerged as a promising avenue in the fight against ovarian cancer, harnessing the body’s immune system to recognize and attack cancer cells. Unlike traditional treatments that directly target tumor cells, immunotherapy aims to enhance the immune response against malignancies. One of the most widely studied forms of immunotherapy in ovarian cancer is immune checkpoint inhibitors, which block proteins that inhibit immune responses.
Agents such as pembrolizumab and nivolumab have shown potential in clinical trials, particularly in patients with high tumor mutational burden or specific biomarkers like PD-L1 expression. In addition to checkpoint inhibitors, other immunotherapeutic strategies are being explored, including therapeutic vaccines and adoptive cell transfer. For example, vaccines designed to elicit a robust immune response against specific tumor antigens are being tested in various clinical settings.
Furthermore, chimeric antigen receptor (CAR) T-cell therapy is being investigated for its ability to engineer a patient’s T-cells to target ovarian cancer cells more effectively. These innovative approaches aim not only to improve survival rates but also to provide durable responses that can lead to long-term remission.
Advancements in Early Detection and Screening
Early detection of ovarian cancer is crucial for improving prognosis and survival rates; however, the lack of effective screening methods has historically posed significant challenges. Traditional imaging techniques and tumor markers like CA-125 have limitations in sensitivity and specificity, often leading to late-stage diagnoses. Recent advancements in biomarker research and imaging technologies are paving the way for more effective screening strategies.
For instance, researchers are investigating novel blood-based biomarkers that could provide earlier indications of ovarian cancer presence. One promising area of research involves the use of multi-omics approaches that integrate genomic, proteomic, and metabolomic data to identify unique signatures associated with early-stage ovarian cancer. These signatures could potentially lead to the development of non-invasive screening tests that can detect the disease at a much earlier stage than currently possible.
Additionally, advancements in imaging techniques such as MRI and ultrasound are being refined to enhance their diagnostic accuracy. Clinical trials focusing on these innovative screening methods are essential for determining their effectiveness in real-world settings and could significantly alter the landscape of ovarian cancer management.
Clinical Trials and Innovative Treatment Approaches
| Trial Name | Phase | Number of Participants | Intervention | Primary Outcome | Status |
|---|---|---|---|---|---|
| OVAR-3 | Phase III | 800 | Paclitaxel + Carboplatin | Progression-Free Survival | Completed |
| GOG-0218 | Phase III | 1200 | Bevacizumab + Chemotherapy | Overall Survival | Completed |
| SOLO-1 | Phase III | 391 | Olaparib Maintenance | Progression-Free Survival | Completed |
| PAOLA-1 | Phase III | 806 | Olaparib + Bevacizumab | Progression-Free Survival | Completed |
| ENGOT-OV16/NOVA | Phase III | 553 | Niraparib Maintenance | Progression-Free Survival | Completed |
| ICON8 | Phase III | 1566 | Weekly vs. 3-weekly Chemotherapy | Progression-Free Survival | Completed |
Clinical trials serve as the backbone of medical research, providing a structured framework for evaluating new treatments and interventions. In the context of ovarian cancer, these trials are critical for assessing innovative treatment approaches that may offer hope where conventional therapies have failed. For example, combination therapies that integrate chemotherapy with targeted agents or immunotherapies are being rigorously tested in clinical settings.
Such trials aim to determine optimal dosing schedules, assess safety profiles, and evaluate overall efficacy compared to standard treatment regimens. Moreover, adaptive trial designs are gaining traction in oncology research, allowing for modifications based on interim results without compromising scientific integrity. This flexibility can accelerate the development process for promising therapies while ensuring patient safety.
Trials that incorporate real-time data analysis can quickly identify which treatment arms are most effective, enabling researchers to pivot strategies as needed. The ongoing exploration of innovative treatment modalities through clinical trials is vital for advancing care standards and improving outcomes for patients with ovarian cancer.
The Role of Genetic Testing in Ovarian Cancer Trials
Genetic testing plays a pivotal role in the management of ovarian cancer, particularly in identifying hereditary syndromes such as BRCA mutations that significantly increase a woman’s risk for developing the disease. The integration of genetic testing into clinical trials has transformed our understanding of ovarian cancer biology and treatment response. By identifying patients with specific genetic alterations, researchers can tailor therapies that target these vulnerabilities more effectively.
For instance, women with BRCA mutations may benefit from PARP inhibitors due to their compromised DNA repair capabilities. Clinical trials focusing on these targeted therapies often include genetic testing as a prerequisite for enrollment, ensuring that participants are selected based on their tumor’s molecular profile. Additionally, genetic testing can inform risk-reducing strategies for at-risk individuals, guiding decisions regarding prophylactic surgeries or enhanced surveillance protocols.
As genetic testing becomes more accessible and comprehensive, its incorporation into clinical trials will continue to shape personalized treatment approaches for ovarian cancer.
Promising Results and Future Directions
The landscape of ovarian cancer research is marked by a series of promising results emerging from clinical trials that have the potential to reshape treatment paradigms. For instance, recent studies have demonstrated improved progression-free survival rates with the use of novel combinations of targeted therapies and immunotherapies compared to traditional chemotherapy alone. These findings underscore the importance of continued investment in research aimed at understanding the complex biology of ovarian cancer and identifying effective therapeutic strategies.
Looking ahead, future directions in ovarian cancer research will likely focus on refining existing treatments while exploring novel agents that target previously unaddressed pathways. The integration of artificial intelligence and machine learning into clinical trial design may also enhance patient stratification and optimize treatment selection based on individual tumor characteristics. Furthermore, ongoing collaborations between academic institutions, pharmaceutical companies, and patient advocacy groups will be crucial for accelerating the development of innovative therapies and ensuring that advancements translate into meaningful benefits for patients.
Patient Perspectives and Advocacy in Ovarian Cancer Trials
The voices of patients play an integral role in shaping the landscape of ovarian cancer research and clinical trials. Patient advocacy groups have emerged as powerful allies in raising awareness about the disease, promoting research funding, and ensuring that patient needs are prioritized in trial designs. These organizations often provide invaluable resources for patients navigating their treatment options while also advocating for greater access to clinical trials.
Moreover, incorporating patient perspectives into trial design can enhance recruitment efforts and improve retention rates by addressing barriers that may prevent participation. Engaging patients in discussions about trial objectives, potential risks, and expected outcomes fosters a sense of ownership over their treatment journey. As more patients become informed advocates for their health care choices, their contributions will continue to drive progress in ovarian cancer research and ensure that future trials align with patient-centered goals.
In conclusion, the ongoing evolution of ovarian cancer trials reflects a commitment to improving outcomes through innovative research approaches. By embracing targeted therapies, immunotherapy, early detection methods, genetic testing, and patient advocacy, the field is poised for significant advancements that could transform the lives of those affected by this challenging disease.




