Prostate cancer remains one of the most prevalent malignancies among men worldwide, with millions diagnosed each year. The complexity of this disease, characterized by its heterogeneous nature and varying degrees of aggressiveness, necessitates ongoing research and clinical trials to develop effective treatment strategies. Clinical trials serve as a critical bridge between laboratory discoveries and patient care, providing a structured environment to evaluate new therapies, assess their safety and efficacy, and ultimately improve patient outcomes.
These trials are essential not only for testing novel drugs but also for exploring innovative treatment combinations and refining existing protocols. The landscape of prostate cancer trials has evolved significantly over the past few decades, driven by advancements in molecular biology and a deeper understanding of tumor biology. Researchers are increasingly focused on personalized medicine approaches that tailor treatments based on individual patient characteristics, including genetic profiles and tumor markers.
This shift towards precision medicine is reflected in the design of contemporary clinical trials, which often incorporate biomarker-driven strategies to identify patients who are most likely to benefit from specific therapies. As a result, the ongoing research in prostate cancer trials is not only expanding the arsenal of treatment options but also enhancing the quality of life for patients through more targeted interventions.
Key Takeaways
- Prostate cancer trials are essential for developing and evaluating new treatment strategies.
- Emerging treatments include targeted therapies and immunotherapy to improve patient outcomes.
- Advances in early detection and precision medicine are enhancing diagnosis and personalized care.
- Clinical trials play a critical role in prostate cancer research and the approval of innovative therapies.
- Future directions focus on integrating novel approaches to optimize treatment efficacy and patient quality of life.
New Treatment Options for Prostate Cancer
The development of new treatment options for prostate cancer has been a focal point of research in recent years, particularly as resistance to traditional therapies becomes more common. Hormonal therapies, such as androgen deprivation therapy (ADT), have long been the cornerstone of treatment for advanced prostate cancer. However, the emergence of novel agents like enzalutamide and abiraterone has transformed the therapeutic landscape.
These drugs target androgen receptor signaling pathways more effectively than previous treatments, leading to improved survival rates and quality of life for patients with metastatic castration-resistant prostate cancer (mCRPC). In addition to hormonal therapies, chemotherapy has also seen significant advancements. Docetaxel was the first chemotherapy agent shown to improve survival in metastatic prostate cancer, but newer agents like cabazitaxel have emerged as effective alternatives for patients who have progressed after docetaxel treatment.
Furthermore, the introduction of radium-223, a radiopharmaceutical that selectively targets bone metastases, has provided a novel approach to managing symptomatic bone pain while extending survival in patients with bone-dominant disease. These new treatment options underscore the importance of continuous research and clinical trials in identifying therapies that can offer better outcomes for patients with prostate cancer.
Targeted Therapies in Prostate Cancer Trials

Targeted therapies represent a paradigm shift in the treatment of prostate cancer, focusing on specific molecular targets associated with tumor growth and progression. One of the most promising areas of research involves the identification of genetic mutations that drive prostate cancer development. For instance, mutations in the BRCA1 and BRCA2 genes, commonly associated with breast and ovarian cancers, have been found in a subset of prostate cancer patients.
This discovery has led to the exploration of PARP inhibitors, such as olaparib and rucaparib, which exploit the DNA repair deficiencies caused by these mutations. Clinical trials investigating targeted therapies are increasingly incorporating biomarker selection to enhance patient stratification. For example, studies have shown that patients with tumors harboring specific alterations in the PI3K/AKT/mTOR pathway may respond better to inhibitors targeting this pathway.
The use of next-generation sequencing (NGS) technologies has facilitated the identification of these actionable mutations, allowing researchers to design trials that test targeted agents in genetically defined populations. This approach not only maximizes the potential for therapeutic success but also minimizes unnecessary exposure to ineffective treatments.
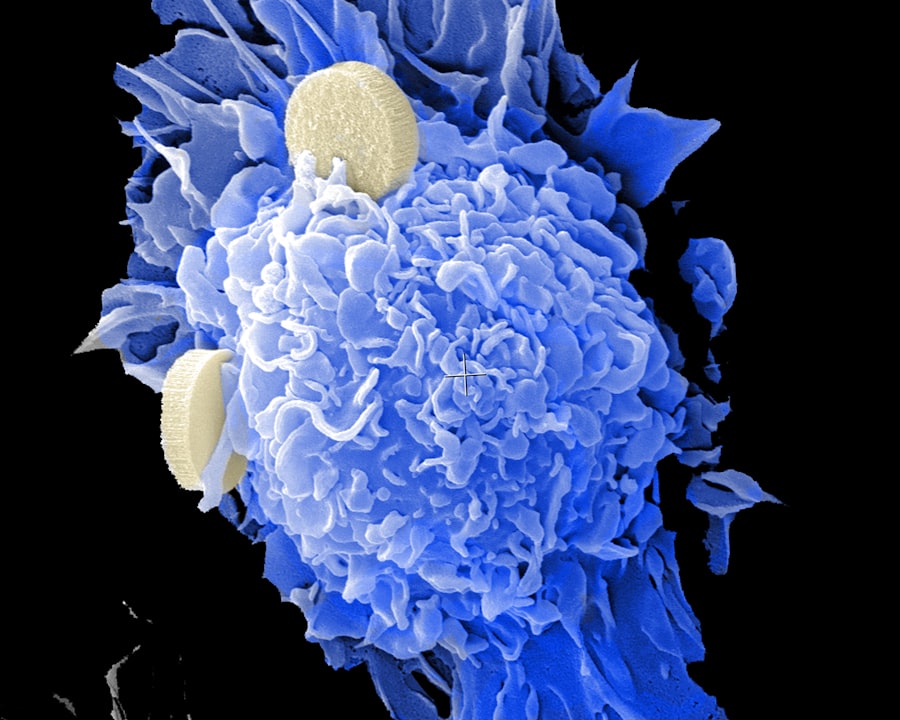
Immunotherapy and Prostate Cancer
Immunotherapy has emerged as a revolutionary approach in oncology, harnessing the body’s immune system to combat cancer cells. In prostate cancer, several immunotherapeutic strategies are currently under investigation. One of the most notable is sipuleucel-T, an autologous cellular therapy designed to stimulate an immune response against prostatic acid phosphatase (PAP), a protein expressed in many prostate cancers.
Clinical trials have demonstrated that sipuleucel-T can extend survival in asymptomatic or minimally symptomatic metastatic castration-resistant prostate cancer patients. Another promising avenue is the use of immune checkpoint inhibitors, which have transformed treatment paradigms in various malignancies by blocking proteins that inhibit immune responses. While prostate cancer has historically been considered less immunogenic than other cancers, ongoing trials are exploring combinations of checkpoint inhibitors with other modalities, such as hormonal therapy or radiation therapy, to enhance their efficacy.
For instance, studies are investigating the combination of pembrolizumab with ADT in patients with high-risk localized disease, aiming to improve outcomes by unleashing a more robust immune response against tumor cells.
Advancements in Early Detection and Diagnosis
| Trial Name | Phase | Number of Participants | Intervention | Primary Outcome | Status |
|---|---|---|---|---|---|
| PROSPER | Phase 3 | 1401 | Enzalutamide + ADT | Metastasis-free survival | Completed |
| SPARTAN | Phase 3 | 1207 | Apalutamide + ADT | Metastasis-free survival | Completed |
| IPATential150 | Phase 3 | 525 | Ipatasertib + Abiraterone | Radiographic progression-free survival | Completed |
| STAMPEDE | Phase 3 | 2962 | Multiple arms (ADT +/- other agents) | Overall survival | Ongoing |
| CHAARTED | Phase 3 | 790 | Docetaxel + ADT | Overall survival | Completed |
Early detection of prostate cancer is crucial for improving treatment outcomes and survival rates. Traditional screening methods, such as prostate-specific antigen (PSA) testing, have been instrumental in identifying cases at an earlier stage; however, they are not without limitations, including false positives and overdiagnosis. Recent advancements in diagnostic technologies have led to the development of more refined biomarkers and imaging techniques that enhance early detection capabilities.
One significant advancement is the use of multiparametric magnetic resonance imaging (mpMRI), which provides detailed images of the prostate and surrounding tissues. This imaging modality allows for better localization of tumors and can guide biopsies more accurately than traditional methods. Clinical trials are currently evaluating the role of mpMRI in active surveillance protocols, aiming to reduce unnecessary interventions while ensuring that clinically significant cancers are not missed.
Additionally, liquid biopsy techniques that analyze circulating tumor DNA (ctDNA) are being explored as non-invasive methods for early detection and monitoring disease progression.
Precision Medicine in Prostate Cancer Trials
Precision medicine represents a transformative approach to cancer treatment that tailors therapies based on individual patient characteristics, including genetic makeup and tumor biology. In prostate cancer trials, this concept is gaining traction as researchers seek to identify specific biomarkers that predict response to various treatments. The integration of genomic profiling into clinical practice has enabled oncologists to select therapies that align with the unique molecular features of each patient’s tumor.
For instance, genomic tests such as Oncotype DX and Decipher provide insights into the aggressiveness of prostate cancer and help guide treatment decisions for localized disease. These tests analyze gene expression patterns to predict outcomes and inform whether patients may benefit from additional therapies post-surgery or radiation. Ongoing clinical trials are further investigating how these genomic insights can be utilized to optimize treatment regimens and improve patient stratification in both localized and advanced disease settings.
Clinical Trials and Prostate Cancer Research
Clinical trials are fundamental to advancing our understanding of prostate cancer and developing new therapeutic strategies. They provide a structured framework for evaluating new treatments while ensuring patient safety through rigorous monitoring and ethical oversight. The National Cancer Institute (NCI) and various pharmaceutical companies sponsor numerous clinical trials aimed at exploring innovative therapies, combinations, and treatment modalities.
Participation in clinical trials offers patients access to cutting-edge treatments that may not yet be available through standard care pathways. Moreover, these trials often include comprehensive data collection on patient outcomes, side effects, and quality of life measures, contributing valuable information to the broader scientific community. For example, large-scale phase III trials comparing novel agents against standard-of-care treatments have been pivotal in establishing new standards for managing advanced prostate cancer.
Future Directions in Prostate Cancer Trials
The future of prostate cancer trials is poised for exciting developments as researchers continue to explore novel therapeutic avenues and refine existing strategies. One promising direction is the integration of artificial intelligence (AI) and machine learning into clinical trial design and patient management. These technologies can analyze vast datasets to identify patterns that may inform treatment decisions or predict patient responses based on genetic profiles.
Additionally, there is a growing emphasis on combination therapies that leverage multiple mechanisms of action to overcome resistance and enhance efficacy. For instance, combining immunotherapy with targeted therapies or radiation may yield synergistic effects that improve outcomes for patients with advanced disease. As our understanding of tumor microenvironments deepens, future trials will likely focus on optimizing treatment regimens based on individual tumor characteristics and immune profiles.
Furthermore, global collaboration among researchers, institutions, and pharmaceutical companies will be essential in accelerating progress in prostate cancer research. Initiatives aimed at sharing data across platforms can facilitate larger-scale studies that enhance statistical power and lead to more robust conclusions about treatment efficacy. As we move forward into an era defined by precision medicine and innovative therapeutic strategies, clinical trials will remain at the forefront of efforts to combat prostate cancer effectively.