This article examines the ongoing progress of antisense oligonucleotides (ASOs) in clinical trials, highlighting their evolving therapeutic potential and the challenges that remain. ASOs are short, synthetic strands of nucleic acids designed to interfere with gene expression at the RNA level. They act like molecular keys, selectively binding to messenger RNA (mRNA) molecules and either degrading them or blocking their translation into proteins. This targeted approach offers a way to address diseases caused by specific genetic faults or aberrant protein production.
The concept of modulating gene expression using nucleic acids has a long scientific lineage. Early research into antisense technology, dating back several decades, laid the groundwork for the development of ASOs. These initial efforts, while conceptually sound, faced significant hurdles. Delivery to target cells, stability within the body, and potential off-target effects were major concerns that researchers worked to overcome. The advent of modified nucleotides and improved delivery strategies proved instrumental in transforming theoretical promise into tangible therapeutic potential.
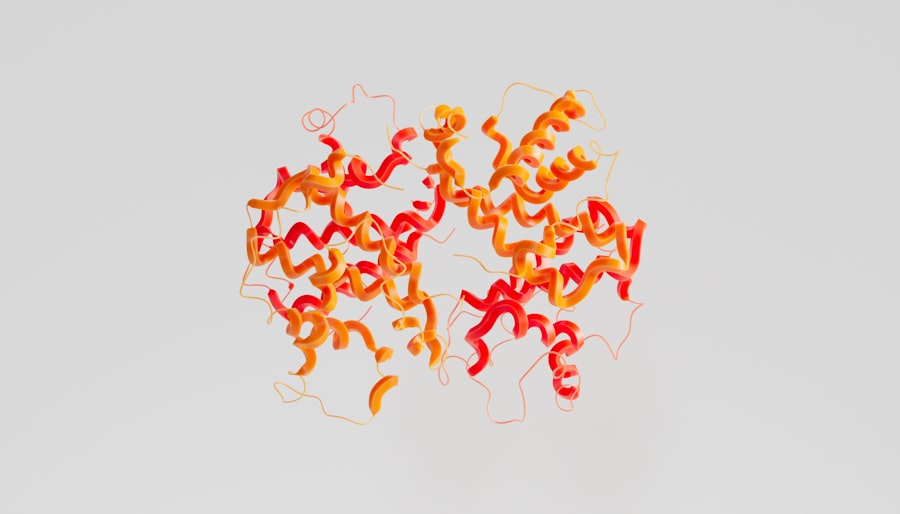
The Mechanism of Action: A Molecular Intervention
ASOs function through several primary mechanisms. The most common is RNase H-mediated degradation, where the ASO binds to its target mRNA, forming a DNA-RNA hybrid. This hybrid then recruits a cellular enzyme called RNase H, which cleaves the mRNA, preventing protein synthesis. Other mechanisms include steric blocking, where the ASO physically obstructs the ribosome’s passage along the mRNA, and modulation of RNA splicing. By precisely targeting the genetic instructions for protein production, ASOs offer a refined approach to treating disease.
The Genetic Blueprint: Targeting Disease at its Root
Many diseases have their origins in errors within an individual’s genetic code, leading to the production of faulty proteins or a lack of essential ones. ASOs offer a unique advantage by directly addressing these genetic underpinnings. Instead of managing symptoms or broadly inhibiting cellular processes, ASOs can be designed to silence the specific gene responsible for the disease pathology. This precision is akin to a surgeon performing a delicate operation versus a general practitioner treating a broad range of ailments.
Navigating the Clinical Trial Landscape
The journey from laboratory discovery to approved medicine is arduous, marked by rigorous phases of clinical investigation. ASOs have traversed this landscape with increasing success, demonstrating their therapeutic efficacy in a growing number of indications. Clinical trials for ASOs have progressed from early-stage safety and feasibility studies to large-scale efficacy trials, offering a glimpse into their future impact on healthcare.
Phase 1 Trials: Safety First
The initial stages of ASO clinical development focus on establishing safety and tolerability in human subjects. These trials typically involve a small number of healthy volunteers or patients with advanced disease. Researchers meticulously monitor for adverse events and determine the maximum tolerated dose. This foundational step is crucial, as even the most promising therapeutic agent must first prove it can be administered safely.
Phase 2 Trials: Early Efficacy Signals
Once safety is established, Phase 2 trials delve into assessing the preliminary efficacy of an ASO. These studies involve a larger patient population with the target disease and are designed to collect data on whether the ASO produces the intended therapeutic effect. Dose-ranging studies are often conducted to identify the optimal dosage for subsequent trials. Positive signals in Phase 2 trials are critical inflection points, suggesting the ASO warrants further investigation.
Phase 3 Trials: Definitive Efficacy and Comparison
Phase 3 trials represent the most extensive and critical stage of clinical evaluation. These trials involve hundreds or even thousands of patients and aim to definitively demonstrate the ASO’s efficacy and safety in comparison to a placebo or standard of care. Rigorous statistical analysis is employed to confirm therapeutic benefit. Successful completion of Phase 3 trials is a prerequisite for seeking regulatory approval from agencies such as the U.S. Food and Drug Administration (FDA) or the European Medicines Agency (EMA).
Expanding Therapeutic Horizons: Approved Therapies and Emerging Indications

The successful translation of ASO technology into approved therapies has opened doors to treating a range of previously intractable diseases. This success fuels further research into new applications, widening the spectrum of conditions that ASOs may address.
Spinal Muscular Atrophy (SMA): A Landmark Achievement
One of the most significant breakthroughs for ASOs has been in the treatment of Spinal Muscular Atrophy (SMA). This devastating genetic disorder affects motor neurons, leading to progressive muscle weakness and atrophy. Nusinersen, an ASO, was the first treatment approved for SMA, demonstrating the ability to significantly improve motor function and survival in affected individuals. This approval served as a powerful validation of ASO technology.
Hereditary Transthyretin Amyloidosis (hATTR Amyloidosis): Targeting Protein Misfolding
Another area where ASOs have made a substantial impact is in the treatment of hereditary transthyretin amyloidosis (hATTR amyloidosis). This condition is caused by mutations in the TTR gene, leading to the production of misfolded transthyretin protein that deposits in various organs, causing severe damage. Patisiran and inotersen, both ASOs, are approved to reduce the production of this misfolded protein, offering a lifeline to patients.
Other Neurological Disorders: Unlocking Potential
Beyond SMA and hATTR amyloidosis, ASO therapies are showing promise in a variety of other neurological disorders. Research is actively exploring their use in conditions such as Huntington’s disease, amyotrophic lateral sclerosis (ALS), and various rare genetic neuropathies. The ability of ASOs to cross the blood-brain barrier and target specific genes within neurons is a key factor in their investigation for these complex conditions.
Overcoming Challenges: The Road Ahead
Despite the significant advancements, challenges remain in the widespread and optimized application of ASO therapies. Addressing these hurdles is essential for unlocking the full potential of this therapeutic modality.
Delivery Enigmas: Reaching the Target
The effective delivery of ASOs to their intended cellular targets remains a critical area of research. While some ASOs can be administered intravenously or intrathecally (into the spinal fluid), reaching all necessary tissues, particularly solid organs, can be challenging. Strategies such as chemical modifications of the oligonucleotide, conjugation with targeting ligands, and the development of advanced nanoparticle delivery systems are under active investigation to improve tissue penetration and cellular uptake.
Selectivity and Off-Target Effects: Precision is Paramount
Ensuring that ASOs bind only to their intended mRNA targets and avoid unintended interactions is crucial for minimizing side effects. While ASOs are designed for high specificity, it is essential to conduct thorough preclinical and clinical evaluations to identify and mitigate any potential off-target effects. Ongoing research focuses on optimizing ASO design and sequence selection to enhance selectivity.
Immunogenicity and Long-Term Safety: A Vigilant Watch
As with any therapeutic intervention, the potential for immunogenicity – the body’s response to the ASO itself – is a consideration. While current ASO therapies have generally demonstrated good tolerability, long-term safety data from ongoing and future trials will be vital in fully understanding any potential immunological responses. Continuous monitoring and post-market surveillance are integral to ensuring patient safety.
Cost and Accessibility: Bridging the Divide
The development of novel therapeutics, particularly those involving complex manufacturing processes like ASOs, often comes with significant costs. Ensuring that these life-changing treatments are accessible to all patients who can benefit from them is a societal challenge that requires multifaceted solutions. Collaboration between manufacturers, payers, and patient advocacy groups will be key to addressing these economic realities.
The Future Trajectory: Innovation and Expansion
| Trial Phase | Number of Trials | Target Diseases | Common Delivery Methods | Primary Outcome Measures | Estimated Completion Year |
|---|---|---|---|---|---|
| Phase 1 | 25 | Duchenne Muscular Dystrophy, Spinal Muscular Atrophy | Intrathecal, Intravenous | Safety, Tolerability | 2024-2025 |
| Phase 2 | 18 | Huntington’s Disease, Amyotrophic Lateral Sclerosis | Intrathecal, Subcutaneous | Efficacy, Dose Optimization | 2025-2026 |
| Phase 3 | 10 | Familial Hypercholesterolemia, Hereditary Transthyretin Amyloidosis | Intravenous, Subcutaneous | Long-term Efficacy, Safety | 2026-2027 |
| Completed | 15 | Various Rare Genetic Disorders | Multiple | Safety, Efficacy | 2023-2024 |
The field of antisense oligonucleotide therapy is dynamic, with ongoing innovation promising to expand its reach and refine its application. Research is continually pushing the boundaries of what is possible, suggesting a bright future for this elegant therapeutic approach.
Next-Generation ASOs: Enhanced Properties
The development of next-generation ASOs is a key focus. These advancements aim to improve properties such as potency, bioavailability, cellular uptake, and tissue distribution. Researchers are exploring novel chemical modifications, alternative backbone structures, and innovative conjugation strategies to create ASOs with superior therapeutic profiles. This iterative process of refinement is akin to a craftsman continually sharpening their tools for greater precision.
Expanding the Disease Portfolio: From Rare to Common
While ASOs have initially found success in rare genetic diseases, there is significant interest in their application to more prevalent conditions. Research is exploring the potential of ASOs in areas such as cardiovascular disease, metabolic disorders, and infectious diseases. The ability to target specific causal pathways offers a new paradigm for treating a broader spectrum of human ailments.
Combination Therapies: Synergistic Power
The potential for combining ASOs with other therapeutic modalities is another exciting frontier. For certain complex diseases, a single intervention may not be sufficient. Combining ASOs with gene therapy, small molecule drugs, or other biological agents could lead to synergistic effects, offering enhanced efficacy and improved patient outcomes. This approach is like a symphony, where different instruments come together to create a richer, more complex sound.
Conclusion: A Transformative Class of Therapeutics
Antisense oligonucleotides represent a transformative class of therapeutics, offering a precise and targeted approach to treating a growing range of diseases. The progress witnessed in clinical trials, from early safety assessments to the approval of life-altering treatments for conditions like SMA and hATTR amyloidosis, underscores the immense potential of this technology. While challenges related to delivery, selectivity, and cost persist, ongoing innovation and dedicated research are steadily paving the way for ASOs to become an even more integral part of the therapeutic armamentarium, offering hope and improved outcomes for patients worldwide. The current trajectory suggests that ASO therapy is not merely a passing trend but a fundamental shift in how we approach the treatment of genetic and RNA-driven diseases.