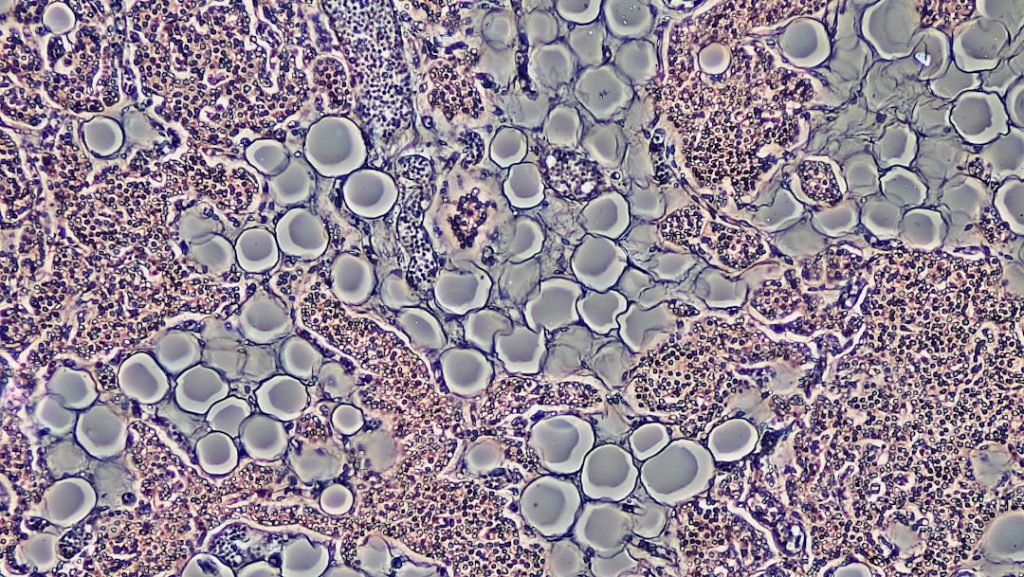
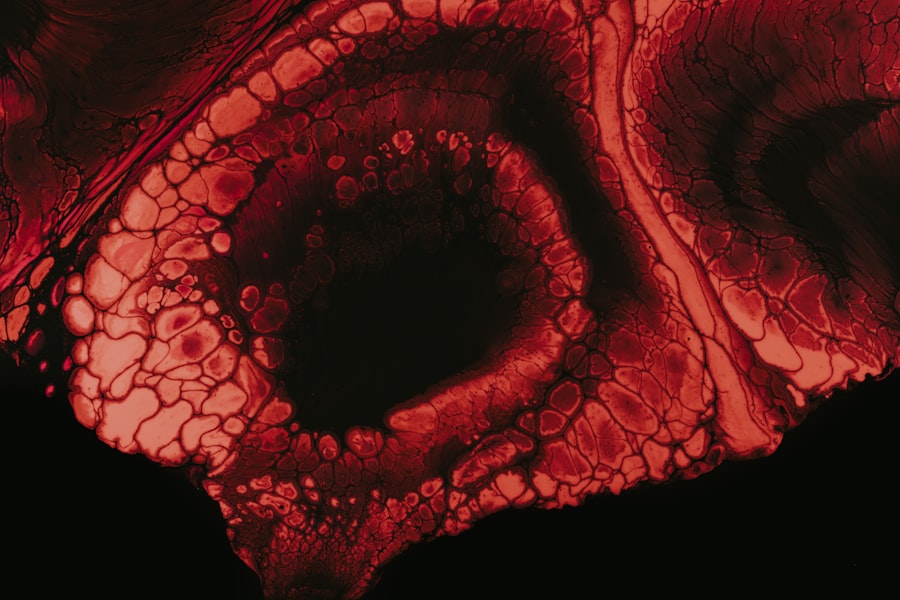
Multiple myeloma is a complex and often challenging hematological malignancy characterized by the proliferation of abnormal plasma cells in the bone marrow. These malignant plasma cells disrupt normal blood cell production, leading to a range of complications, including anemia, increased susceptibility to infections, and bone lesions. The disease is often insidious in its onset, with many patients experiencing vague symptoms such as fatigue, bone pain, or recurrent infections before receiving a definitive diagnosis.
The pathophysiology of multiple myeloma involves a series of genetic mutations and microenvironmental changes that allow these malignant cells to thrive and evade the immune system. The disease is classified into several subtypes based on genetic and molecular characteristics, which can influence prognosis and treatment response. For instance, patients with high-risk cytogenetic abnormalities, such as del(17p) or t(4;14), may have a more aggressive disease course and poorer outcomes compared to those with standard-risk features.
The International Staging System (ISS) is commonly used to assess the severity of the disease, taking into account factors such as serum beta-2-microglobulin and albumin levels. Understanding these nuances is crucial for tailoring treatment strategies and improving patient outcomes.
Key Takeaways
- Multiple myeloma is a complex blood cancer requiring diverse treatment approaches.
- Current treatments include chemotherapy, stem cell transplants, and targeted therapies but face significant challenges.
- The Master Trial Myeloma is a novel clinical trial aiming to personalize and improve treatment strategies.
- Patient eligibility for the trial is based on specific criteria to optimize outcomes and safety.
- The trial has the potential to significantly advance future multiple myeloma treatments by tailoring therapies to individual patient profiles.
Current Treatment Options for Multiple Myeloma
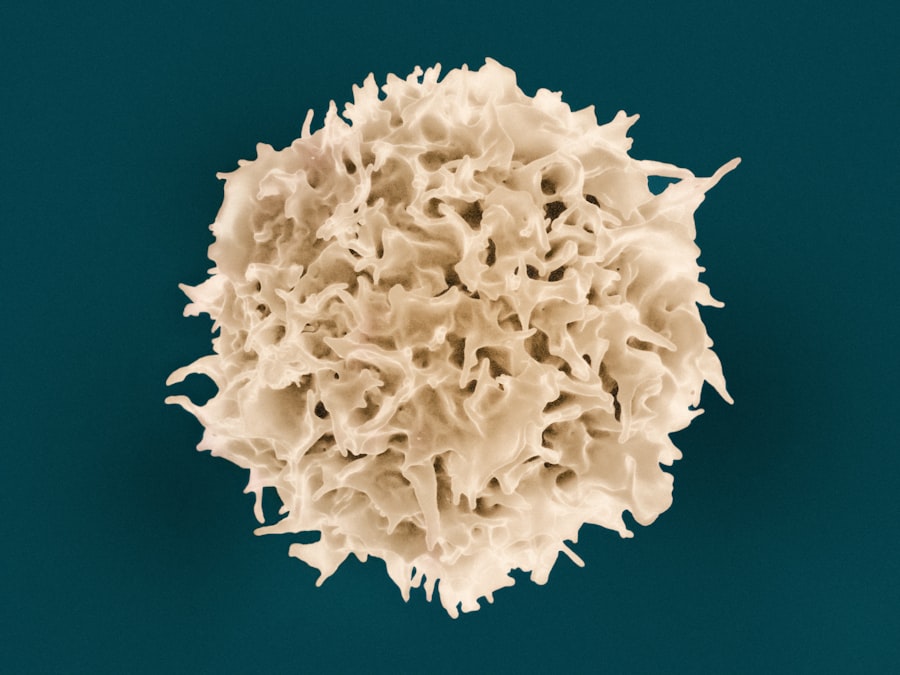
The treatment landscape for multiple myeloma has evolved significantly over the past two decades, with the introduction of novel agents that have transformed patient management. Traditional therapies included alkylating agents like melphalan and corticosteroids, but the advent of immunomodulatory drugs (IMiDs) such as thalidomide, lenalidomide, and pomalidomide has revolutionized treatment paradigms. These agents work by enhancing the immune response against myeloma cells and disrupting their growth signals.
For instance, lenalidomide has become a cornerstone of therapy, often used in combination with dexamethasone or other agents to improve response rates. Proteasome inhibitors, such as bortezomib and carfilzomib, represent another class of drugs that have shown significant efficacy in treating multiple myeloma. By inhibiting the proteasome, these agents induce apoptosis in malignant plasma cells and have been integrated into various treatment regimens.
Additionally, monoclonal antibodies like daratumumab and isatuximab target specific surface markers on myeloma cells, providing a new avenue for therapy. These agents can be used in both relapsed and newly diagnosed settings, often in combination with other therapies to enhance their effectiveness.
Challenges in Treating Multiple Myeloma
Despite the advancements in treatment options, multiple myeloma remains a challenging disease to manage due to its heterogeneity and the development of drug resistance. One of the primary challenges is the emergence of resistant clones that can survive even in the presence of effective therapies. This phenomenon complicates treatment regimens and often necessitates a shift to alternative therapies or clinical trial participation.
Moreover, the side effects associated with current treatments can significantly impact patients’ quality of life, leading to treatment discontinuation or dose modifications. Another significant challenge is the need for personalized treatment approaches. Given the diverse genetic landscape of multiple myeloma, what works for one patient may not be effective for another.
This variability underscores the importance of biomarker-driven strategies to identify which patients are likely to benefit from specific therapies. Additionally, access to cutting-edge treatments can be limited by geographic and socioeconomic factors, creating disparities in care that can affect outcomes. Addressing these challenges requires ongoing research and collaboration among healthcare providers, researchers, and patients.
Introduction to Master Trial Myeloma
The Master Trial Myeloma initiative represents a groundbreaking approach to clinical research in multiple myeloma, aiming to streamline the process of evaluating new therapies while providing patients with access to innovative treatments. This adaptive trial design allows for the simultaneous testing of multiple investigational agents within a single framework, thereby accelerating the pace of research and enhancing our understanding of treatment efficacy. By utilizing a master protocol, researchers can efficiently allocate resources and adapt the trial based on emerging data, ultimately leading to more informed decision-making regarding patient care.
One of the key features of the Master Trial Myeloma is its focus on precision medicine. By incorporating biomarker assessments into the trial design, researchers can identify patient subgroups that are more likely to respond to specific therapies. This approach not only enhances the likelihood of successful outcomes but also minimizes exposure to ineffective treatments.
The trial’s structure allows for continuous monitoring and adjustment based on real-time results, making it a dynamic platform for advancing our knowledge of multiple myeloma treatment.
Advancements in Treatment Options through Master Trial Myeloma
| Metric | Description | Value | Unit |
|---|---|---|---|
| Trial Name | Master Trial Myeloma | MASTER | N/A |
| Study Phase | Clinical trial phase | 2 | N/A |
| Patient Population | Number of enrolled patients | 123 | patients |
| Primary Endpoint | Measure of treatment success | MRD negativity rate | percentage |
| MRD Negativity Rate | Minimal residual disease negative after treatment | 80 | % |
| Progression-Free Survival (PFS) | Time without disease progression | 24 | months |
| Overall Survival (OS) | Time from treatment to death from any cause | Not reached | N/A |
| Treatment Regimen | Drugs used in the trial | Daratumumab, Carfilzomib, Lenalidomide, Dexamethasone | N/A |
The Master Trial Myeloma has already begun to yield promising results that could reshape the treatment landscape for multiple myeloma. By facilitating the rapid evaluation of novel agents and combinations, this initiative has enabled researchers to identify effective therapies more quickly than traditional trial designs would allow. For example, early findings from the trial have highlighted the potential of combining existing therapies with new agents that target different pathways involved in myeloma cell survival and proliferation.
Moreover, the adaptive nature of the Master Trial Myeloma allows for real-time modifications based on interim analyses. If a particular treatment arm demonstrates superior efficacy or safety profiles, it can be expanded or prioritized for further investigation while less effective arms can be de-emphasized or closed. This flexibility not only accelerates the development of effective therapies but also ensures that patients receive cutting-edge treatments tailored to their specific disease characteristics.
Patient Eligibility and Participation in Master Trial Myeloma
Participation in the Master Trial Myeloma is designed to be inclusive while ensuring that patients meet specific eligibility criteria that align with the trial’s objectives. Generally, eligible participants include adults diagnosed with multiple myeloma who have received prior treatment or are newly diagnosed. The trial aims to enroll a diverse patient population to better understand how different demographics respond to various therapies.
This inclusivity is crucial for generating data that reflects real-world scenarios and enhances the generalizability of findings. Patients interested in participating must undergo thorough screening processes that include comprehensive medical evaluations and biomarker assessments. These evaluations help determine not only eligibility but also which specific treatment arms may be most appropriate based on individual disease characteristics.
Informed consent is a critical component of participation; patients are provided with detailed information about the trial’s purpose, potential risks, and benefits before making their decision. This emphasis on patient autonomy ensures that individuals are empowered to make choices about their treatment options.
Potential Impact of Master Trial Myeloma on the Future of Multiple Myeloma Treatment
The implications of the Master Trial Myeloma extend far beyond immediate clinical outcomes; they hold promise for fundamentally transforming how multiple myeloma is treated in the future. By establishing a framework for rapid evaluation and adaptation of therapies, this initiative could lead to shorter timelines for bringing effective treatments to market. As new agents are identified through this platform, they can be integrated into standard care more swiftly than traditional trial methodologies would allow.
Furthermore, the focus on precision medicine within the Master Trial Myeloma could pave the way for more personalized treatment approaches in multiple myeloma management. As researchers gather data on how different patient subgroups respond to various therapies, they can refine treatment algorithms that optimize outcomes based on individual characteristics. This shift towards tailored therapies not only enhances efficacy but also minimizes unnecessary side effects associated with ineffective treatments.
The Role of Master Trial Myeloma in Advancing Treatment Options for Multiple Myeloma
The Master Trial Myeloma initiative stands at the forefront of innovation in multiple myeloma research and treatment. By leveraging adaptive trial designs and emphasizing precision medicine, it addresses many of the challenges currently faced in managing this complex disease. As ongoing studies continue to yield valuable insights into effective therapies and patient responses, there is hope for improved outcomes and quality of life for those affected by multiple myeloma.
In an era where personalized medicine is becoming increasingly important, initiatives like Master Trial Myeloma exemplify how collaborative efforts can lead to significant advancements in cancer care. The potential impact on future treatment paradigms cannot be overstated; as we learn more about this disease through innovative research frameworks, we move closer to achieving better survival rates and enhanced quality of life for patients battling multiple myeloma.