Optimizing the flow of medical products from manufacturer to patient is a critical undertaking. The clinical supply chain, as it is known, is a complex network of processes, technologies, and stakeholders that ensures the timely and secure delivery of pharmaceuticals, vaccines, medical devices, and other essential healthcare supplies. Over the past decade, the emphasis on maximizing its efficiency has grown substantially, driven by factors such as rising healthcare costs, increasing regulatory scrutiny, the imperative for patient safety, and the evolving landscape of global health. An efficient clinical supply chain is not merely a logistical advantage; it is a foundational element of effective healthcare delivery, impacting patient outcomes, economic sustainability, and public health resilience.
The inherent complexity of the clinical supply chain stems from its unique demands. Unlike consumer goods, errors in the clinical supply chain can have immediate and severe consequences for individual health. Furthermore, the products themselves are often temperature-sensitive, highly regulated, and possess short shelf lives, requiring specialized handling and transport. The journey from raw material to finished product, through clinical trials, manufacturing, distribution, and ultimately to the patient, involves a multitude of touchpoints, each presenting opportunities for delays, waste, or compromise of product integrity.
To understand how to maximize its efficiency, it is essential to dissect the various components of the clinical supply chain and identify areas for improvement. This involves a multi-pronged approach that addresses technological adoption, process re-engineering, strategic partnerships, and robust data management.
The clinical supply chain encompasses a broad spectrum of activities and entities. It begins with the sourcing of raw materials and active pharmaceutical ingredients (APIs), progresses through the rigorous processes of research and development, navigates the stringent requirements of clinical trials, moves into large-scale manufacturing, and then enters the critical distribution phase. This final stage is further divided into wholesale distribution, hospital and pharmacy dispensing, and direct-to-patient delivery. Each segment presents its own challenges and opportunities for optimization.
Sourcing and Procurement Strategies
The initial step in the supply chain is the acquisition of necessary components. This involves not only the selection of reliable suppliers but also the establishment of transparent and resilient procurement processes.
Supplier Relationship Management
Cultivating strong relationships with suppliers is paramount. This involves open communication, clearly defined quality agreements, and shared risk-mitigation strategies. A collaborative approach ensures that suppliers are aligned with the manufacturer’s objectives for quality, timeliness, and ethical conduct.
Raw Material Quality Control
The integrity of the final product is directly dependent on the quality of its constituent parts. Rigorous testing and validation of all incoming raw materials are essential to prevent downstream issues. This acts as the first line of defense against potential disruptions and the introduction of substandard components.
Research and Development Integration
The efficiency of the supply chain is intrinsically linked to the early stages of product development. Integrating supply chain considerations into R&D can prevent costly redesigns and accelerate market entry.
Early-Stage Supply Chain Planning
By involving supply chain experts from the outset of R&D, potential logistical hurdles can be identified and addressed proactively. This avoids situations where a promising drug or device faces insurmountable supply chain challenges later in its development.
Technology Scouting for Supply Chain Enablement
Identifying and evaluating new technologies that can enhance supply chain visibility, speed, and security during the R&D phase can lay the groundwork for a more efficient future.
Streamlining Manufacturing and Production Processes
The manufacturing phase is a critical bottleneck in the clinical supply chain. Optimizing this process involves not only enhancing production throughput but also ensuring flexibility and responsiveness to demand fluctuations.
Lean Manufacturing Principles
Applying lean manufacturing methodologies, such as Just-In-Time (JIT) inventory management and continuous improvement (Kaizen), can significantly reduce waste and improve efficiency. The goal is to eliminate non-value-added activities, thereby shortening production cycles and lowering costs.
Reducing Production Cycle Times
Analyzing and optimizing each step of the manufacturing process to identify and eliminate inefficiencies can lead to substantial reductions in the time it takes to produce a batch. This requires a granular understanding of each operation.
Minimizing Work-in-Progress (WIP) Inventory
Holding excessive WIP inventory can tie up capital and increase the risk of obsolescence. Implementing strategies to reduce WIP levels can free up resources and improve cash flow.
Advanced Manufacturing Technologies
The adoption of advanced manufacturing technologies can revolutionize production, increasing speed, accuracy, and scalability.
Automation and Robotics
The implementation of automated systems and robotics in manufacturing can improve consistency, reduce human error, and increase production volumes. This is particularly relevant for repetitive or high-precision tasks.
Continuous Manufacturing
Transitioning from batch processing to continuous manufacturing can offer significant advantages in terms of efficiency, quality control, and reduced footprint. This method allows for a steady flow of product rather than discrete batches.
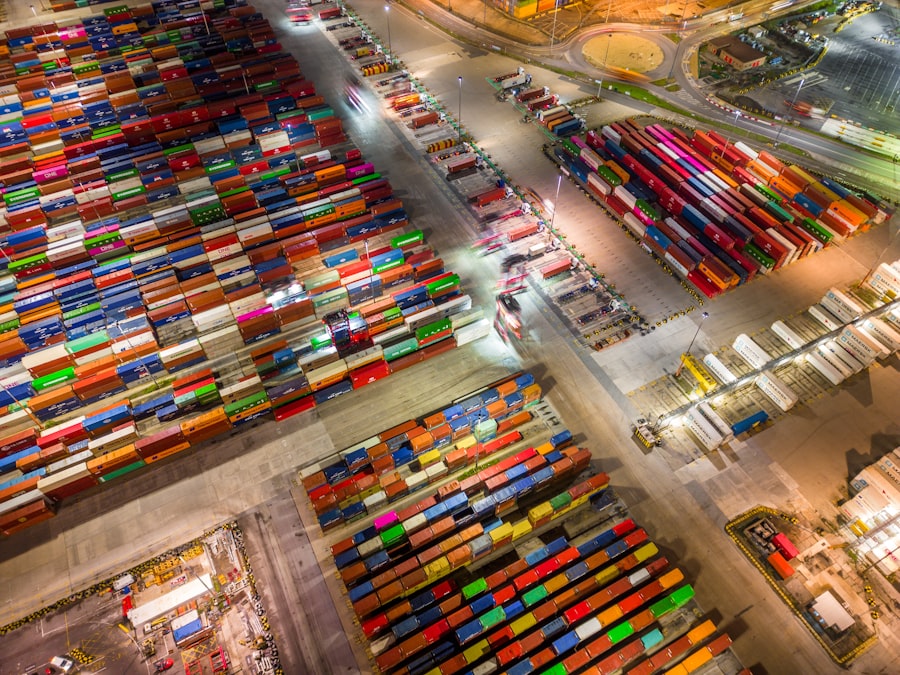
Enhancing Distribution and Logistics Networks
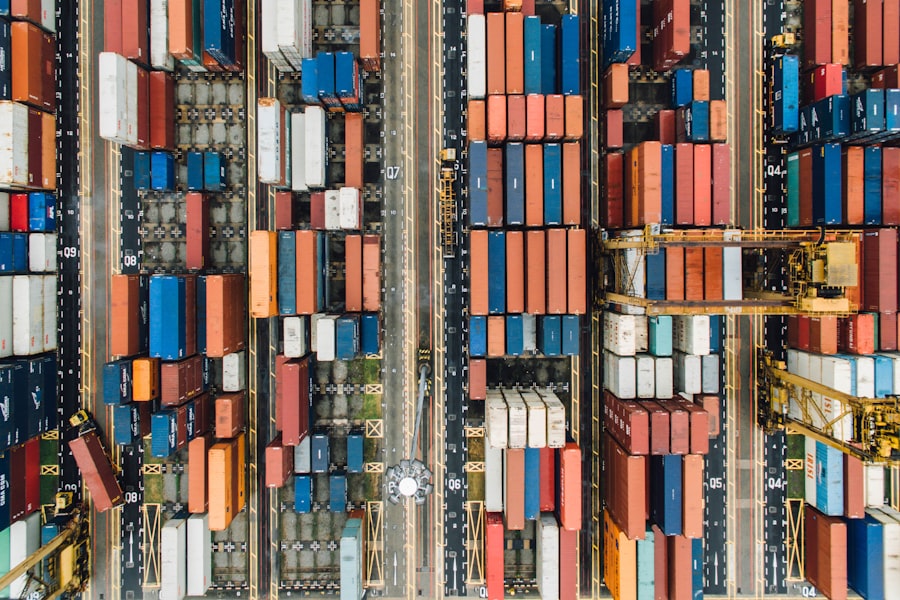
The physical movement of clinical supplies is a complex undertaking. Optimizing distribution channels is crucial for ensuring timely delivery while maintaining product integrity.
Cold Chain Management Excellence
Many clinical products, particularly biologics and vaccines, require stringent temperature control throughout their journey. Maintaining this “cold chain” is a non-negotiable aspect of efficient delivery.
Temperature-Controlled Transportation
Utilizing specialized refrigerated vehicles, passive cooling systems, and active temperature monitoring devices is essential for preserving the efficacy of temperature-sensitive products. This is akin to safeguarding delicate cargo.
Real-Time Temperature Monitoring and Alerts
Implementing advanced tracking systems that provide real-time temperature data and trigger alerts in case of deviations allows for immediate intervention to prevent product spoilage.
Network Optimization and Visibility
Designing and managing distribution networks that are both cost-effective and responsive is key to overall efficiency.
Strategic Warehousing Placement
Strategically locating warehouses closer to points of demand can reduce transit times and associated logistical costs. This requires careful analysis of population density and healthcare facility locations.
Route Optimization Software
Leveraging sophisticated software to plan the most efficient delivery routes, taking into account traffic, delivery windows, and vehicle capacity, can significantly reduce fuel consumption and delivery times.
Last-Mile Delivery Innovations
The final leg of the journey, from a distribution center to a clinic or patient, is often the most challenging. Innovations in this area are crucial.
Direct-to-Patient Shipping Models
For certain medications or devices, direct-to-patient shipping can bypass multiple intermediary steps, potentially reducing costs and improving patient convenience. However, this requires robust tracking and adherence to privacy regulations.
Drone and Autonomous Vehicle Delivery
While still in nascent stages for widespread clinical application, the exploration of drones and autonomous vehicles for last-mile delivery holds promise for remote or time-sensitive deliveries.
Leveraging Technology for Supply Chain Visibility and Control
The integration of technology is fundamental to achieving a high level of efficiency in the clinical supply chain. Visibility into inventory levels, product movement, and potential disruptions is paramount.
Data Analytics and Predictive Modeling
The wealth of data generated throughout the supply chain can be harnessed to gain actionable insights and anticipate future challenges.
Demand Forecasting Accuracy
Utilizing historical data, epidemiological trends, and market intelligence to improve the accuracy of demand forecasts helps prevent stockouts and overstocking. This is like charting a course based on known currents.
Risk Assessment and Mitigation
Analyzing data to identify potential risks, such as supplier insolvency, geopolitical instability, or extreme weather events, allows for the development of proactive mitigation strategies.
Digital Transformation and Integration
Embracing digital tools and integrating disparate systems is crucial for creating a seamless and efficient supply chain.
Enterprise Resource Planning (ERP) Systems
Well-implemented ERP systems can provide a centralized platform for managing all aspects of the supply chain, from procurement to inventory and finance.
Blockchain Technology for Traceability
Blockchain offers a secure and immutable ledger for tracking products, enhancing transparency, and combating counterfeiting. It acts as an unalterable record of every transaction.
Internet of Things (IoT) for Real-Time Monitoring
IoT devices, such as smart sensors and RFID tags, can provide real-time data on product location, environmental conditions, and inventory levels, offering unprecedented visibility.
Fostering Collaboration and Partnerships
| Metric | Description | Typical Value / Benchmark | Impact on Clinical Supply Chain |
|---|---|---|---|
| Inventory Turnover Rate | Number of times inventory is used and replenished over a period | 8-12 times per year | Higher turnover reduces waste and holding costs |
| Order Fulfillment Cycle Time | Time taken from order placement to delivery at clinical site | 3-7 days | Shorter cycle times improve trial timelines and patient access |
| Forecast Accuracy | Degree to which supply forecasts match actual demand | 85-95% | Improves inventory planning and reduces stockouts or overstock |
| Cold Chain Compliance Rate | Percentage of shipments maintained within required temperature ranges | >98% | Ensures drug integrity and regulatory compliance |
| Stockout Rate | Frequency of inventory shortages at clinical sites | Lower stockouts prevent trial delays and patient risk | |
| Waste Rate | Percentage of clinical supplies expired or unusable | Minimizing waste reduces costs and environmental impact | |
| Order Accuracy | Percentage of orders delivered correctly without errors | >99% | Ensures correct supplies reach sites, supporting trial integrity |
No single entity can effectively manage the entire clinical supply chain. Collaboration among all stakeholders is essential for success.
Strategic Alliances and Consortia
Forming partnerships with suppliers, distributors, logistics providers, and even academic institutions can lead to shared resources, knowledge exchange, and joint innovation.
Information Sharing Platforms
Developing secure platforms for sharing relevant information among stakeholders, such as inventory levels, demand forecasts, and potential disruptions, can improve coordination and responsiveness.
Risk and Resilience Planning
Collaboratively developing contingency plans for unforeseen events, such as pandemics or natural disasters, strengthens the overall resilience of the supply chain.
Regulatory Compliance and Engagement
Navigating the complex regulatory landscape is a constant challenge. Proactive engagement with regulatory bodies can ensure compliance and facilitate smoother operations.
Harmonization of Standards
Working towards the harmonization of international regulatory standards can reduce complexity and streamline cross-border movements of clinical supplies.
Stakeholder Education and Training
Ensuring that all individuals involved in the supply chain are adequately trained and understand their roles and responsibilities is crucial for minimizing errors and maximizing efficiency.
Addressing Challenges and Future Trajectories
Despite advancements, the clinical supply chain faces ongoing challenges. These include the increasing complexity of therapies (e.g., personalized medicine), the global nature of manufacturing and distribution, and the constant threat of counterfeiting. Future trajectories involve a greater emphasis on artificial intelligence for predictive analytics, the expansion of advanced manufacturing techniques like 3D printing for on-demand production of certain medical devices, and the continued integration of digital technologies to create a truly connected and intelligent supply chain. The pursuit of maximizing clinical supply chain efficiency is an ongoing journey of continuous improvement, driven by the ultimate goal of ensuring that patients receive the treatments they need, when and where they need them, with unwavering quality and safety.



