Phase 1 clinical trials represent a critical juncture in the drug development process, serving as the first step in evaluating a new therapeutic agent’s safety and pharmacological profile in humans. These trials typically involve a small cohort of healthy volunteers or patients, depending on the nature of the drug being tested. The primary objective is to assess the safety, tolerability, and pharmacokinetics of the investigational drug, laying the groundwork for subsequent phases of clinical research.
The transition from preclinical studies, which often rely on animal models, to human trials is a significant milestone that requires meticulous planning and execution. The design of Phase 1 trials is inherently complex, as it must balance the need for rigorous scientific inquiry with ethical considerations surrounding participant safety. Researchers must navigate regulatory requirements while also ensuring that the trial design is robust enough to yield meaningful data.
This phase often employs various methodologies, including single ascending dose (SAD) and multiple ascending dose (MAD) designs, to systematically evaluate how different doses affect participants. The outcomes of Phase 1 trials not only inform the safety profile of a drug but also provide essential insights into its pharmacodynamics and pharmacokinetics, which are crucial for determining appropriate dosing regimens in later phases.
Key Takeaways
- Phase 1 clinical trials primarily focus on assessing safety, dosage, and pharmacokinetics in a small group of participants.
- Careful trial design, including dose escalation strategies, is crucial to balance safety and efficacy.
- Incorporating biomarkers and pharmacokinetic data enhances understanding of drug behavior and patient response.
- Rigorous patient selection and monitoring of adverse events ensure participant safety and data reliability.
- Emerging innovations and data analysis techniques are shaping the future of more efficient and informative Phase 1 trials.
Key Considerations in Phase 1 Clinical Trial Design
Designing a Phase 1 clinical trial involves several key considerations that can significantly impact the trial’s success. One of the foremost considerations is the selection of an appropriate study population. Depending on the drug’s intended use, researchers may choose to enroll healthy volunteers or patients with specific conditions.
For instance, oncology drugs may be tested in patients with advanced cancer, while other therapeutic areas might prioritize healthy subjects to minimize risk. The choice of population can influence not only safety outcomes but also the generalizability of the trial results. Another critical aspect of Phase 1 trial design is the determination of endpoints.
While safety is the primary endpoint, secondary endpoints may include pharmacokinetic parameters such as maximum concentration (Cmax), time to maximum concentration (Tmax), and area under the curve (AUC). These endpoints help researchers understand how the drug behaves in the body and can inform dose adjustments for subsequent phases. Additionally, the trial design must consider blinding and randomization strategies to minimize bias and enhance the reliability of the data collected.
The incorporation of adaptive designs, which allow for modifications based on interim results, is also gaining traction in Phase 1 trials, providing flexibility in response to emerging data.
Optimizing Dose Escalation Strategies
Dose escalation strategies are pivotal in Phase 1 clinical trials, as they directly influence the assessment of a drug’s safety and efficacy. The goal is to identify the maximum tolerated dose (MTD) while minimizing adverse effects. Traditional dose escalation methods, such as the “3+3” design, involve enrolling three patients at a given dose level and observing for dose-limiting toxicities (DLTs).
If one or more DLTs occur, the trial may either escalate to a higher dose or de-escalate to a lower one based on predefined criteria. However, this conventional approach has limitations, particularly in terms of efficiency and patient exposure to potentially harmful doses. As a result, more innovative strategies have emerged, such as the continual reassessment method (CRM) and Bayesian adaptive designs.
These methodologies allow for more dynamic adjustments to dosing based on real-time data, potentially leading to quicker identification of the MTD and reducing the number of patients exposed to suboptimal doses. For example, CRM uses statistical modeling to predict DLT probabilities at various dose levels, enabling researchers to make informed decisions about dose escalation while maintaining participant safety.
Incorporating Biomarkers and Pharmacokinetics in Phase 1 Trials
The integration of biomarkers into Phase 1 clinical trials has revolutionized how researchers assess drug efficacy and safety. Biomarkers can provide valuable insights into disease mechanisms, treatment responses, and potential adverse effects. For instance, in oncology trials, specific genetic markers may help identify patients who are more likely to benefit from targeted therapies.
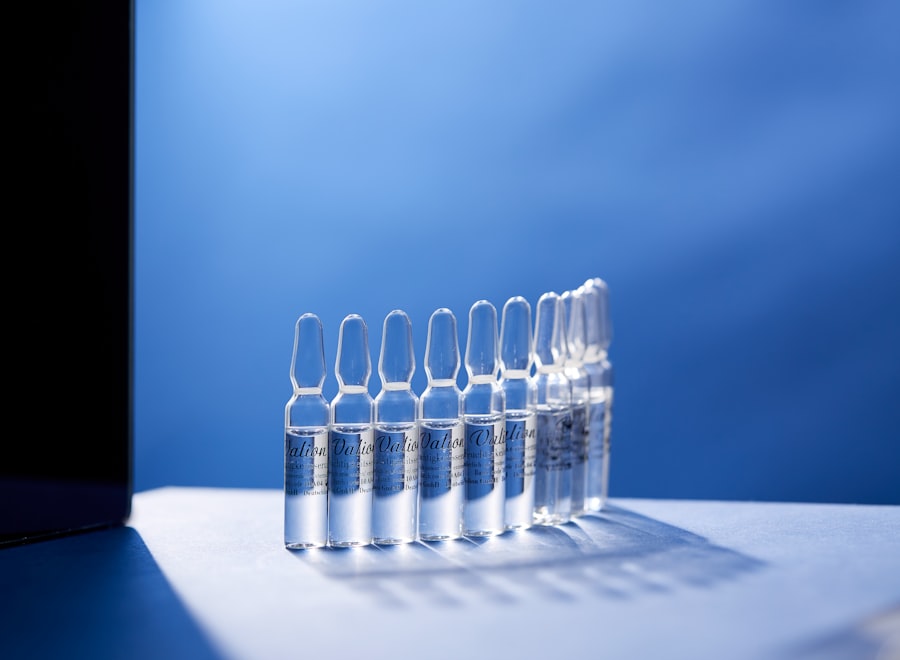
By incorporating biomarker analysis into trial design, researchers can stratify participants based on their likelihood of response, thereby enhancing the precision of the trial outcomes. Pharmacokinetics (PK) is another critical component that must be meticulously evaluated during Phase 1 trials. Understanding how a drug is absorbed, distributed, metabolized, and excreted (ADME) is essential for determining appropriate dosing regimens and predicting potential interactions with other medications.
Advanced analytical techniques such as liquid chromatography-mass spectrometry (LC-MS) enable researchers to obtain detailed PK profiles that inform subsequent phases of development. For example, if a drug exhibits rapid clearance from the body, researchers may need to adjust dosing frequency or explore alternative formulations to maintain therapeutic levels.
Importance of Patient Selection and Inclusion Criteria
| Metric | Description | Typical Range/Value | Purpose |
|---|---|---|---|
| Sample Size | Number of participants enrolled in the trial | 20-80 subjects | To assess safety and tolerability |
| Dose Escalation Scheme | Method for increasing drug dose in cohorts | 3+3 design, accelerated titration, or Bayesian model | To identify maximum tolerated dose (MTD) |
| Primary Endpoint | Main outcome measured to assess safety | Adverse events, dose-limiting toxicities (DLTs) | To evaluate safety profile |
| Secondary Endpoint | Additional outcomes such as pharmacokinetics | Drug concentration in plasma, half-life | To understand drug behavior in the body |
| Inclusion Criteria | Participant characteristics required for enrollment | Healthy volunteers or patients with specific conditions | To select appropriate study population |
| Duration | Length of the clinical trial phase | Several weeks to months | To monitor short-term safety and pharmacokinetics |
| Randomization | Assignment of participants to treatment groups | Often non-randomized or open-label | To simplify safety assessment |
| Blinding | Masking of treatment allocation | Usually open-label; sometimes single-blind | To reduce bias in safety evaluation |
Patient selection is a cornerstone of Phase 1 clinical trials that can significantly influence both safety outcomes and data integrity. Inclusion criteria must be carefully defined to ensure that participants are representative of the target population while also minimizing risks associated with the investigational drug. Factors such as age, sex, comorbidities, and prior treatment history can all impact how a patient responds to a new therapy.
For instance, enrolling older adults in a trial for a novel cardiovascular drug may yield different safety profiles compared to younger populations due to age-related physiological changes. Exclusion criteria are equally important in safeguarding participant welfare and ensuring that trial results are interpretable. Patients with certain pre-existing conditions or those taking specific medications may be excluded to avoid confounding factors that could skew results.
Additionally, ethical considerations surrounding informed consent must be prioritized; participants should fully understand the potential risks and benefits before enrolling in a Phase 1 trial. This emphasis on patient selection not only enhances participant safety but also contributes to the overall validity and reliability of trial outcomes.
Addressing Safety and Adverse Event Monitoring

Safety monitoring is paramount in Phase 1 clinical trials due to the inherent risks associated with testing new drugs in humans for the first time. Adverse events (AEs) must be meticulously tracked and reported throughout the trial duration. Regulatory bodies such as the Food and Drug Administration (FDA) require that all AEs be documented, categorized by severity, and assessed for potential causality related to the investigational drug.
This rigorous monitoring process ensures that any emerging safety concerns are promptly addressed. The implementation of Data Safety Monitoring Boards (DSMBs) plays a crucial role in overseeing participant safety during Phase 1 trials. These independent committees review accumulating data at predetermined intervals to assess whether the trial should continue as planned or if modifications are necessary based on safety concerns.
For example, if a significant number of participants experience severe AEs at a particular dose level, the DSMB may recommend halting further enrollment at that dose or adjusting the study protocol to enhance participant safety. This proactive approach not only protects participants but also upholds the integrity of the research process.
Enhancing Data Collection and Analysis in Phase 1 Trials
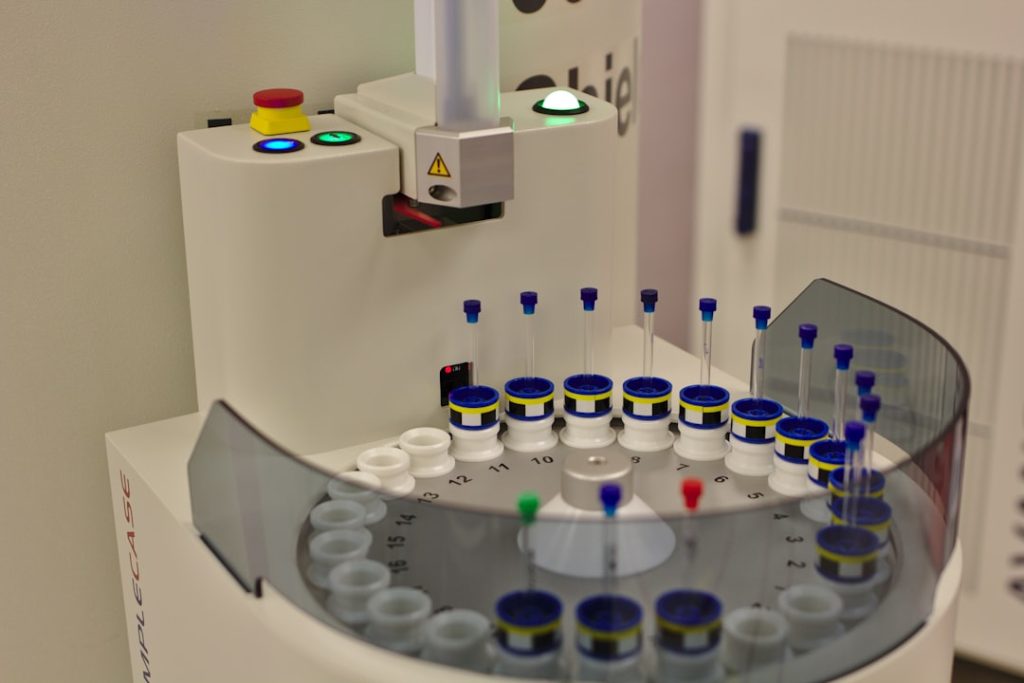
The advancement of technology has significantly enhanced data collection and analysis methodologies in Phase 1 clinical trials. Electronic data capture (EDC) systems have largely replaced traditional paper-based methods, allowing for real-time data entry and monitoring. This shift not only streamlines data management but also reduces errors associated with manual data handling.
Furthermore, EDC systems facilitate remote monitoring by regulatory authorities and sponsors, ensuring compliance with Good Clinical Practice (GCP) guidelines. In addition to improved data collection methods, sophisticated statistical analysis techniques are increasingly employed to derive meaningful insights from trial data. The use of machine learning algorithms and predictive modeling can help identify patterns within complex datasets that may not be apparent through traditional analysis methods.
For instance, these techniques can assist in predicting patient responses based on baseline characteristics or identifying subpopulations that may benefit most from treatment. By leveraging advanced analytics, researchers can enhance their understanding of drug behavior and optimize future trial designs.
Future Trends and Innovations in Phase 1 Clinical Trial Design
As the landscape of clinical research continues to evolve, several trends and innovations are shaping the future of Phase 1 clinical trial design. One notable trend is the increasing emphasis on personalized medicine, which tailors treatments based on individual patient characteristics such as genetics or biomarker profiles. This approach not only enhances treatment efficacy but also minimizes unnecessary exposure to ineffective therapies during early-stage trials.
Another emerging trend is the integration of digital health technologies into clinical trial designs. Wearable devices and mobile health applications enable continuous monitoring of participants’ health metrics outside traditional clinical settings. This real-time data collection can provide valuable insights into drug effects on daily living activities and overall quality of life.
Moreover, virtual trials are gaining traction as they offer greater flexibility for participants while reducing logistical burdens associated with site visits. The incorporation of artificial intelligence (AI) into trial design holds immense potential for optimizing various aspects of Phase 1 studies. AI algorithms can assist in patient recruitment by analyzing electronic health records to identify eligible candidates more efficiently.
Additionally, AI-driven simulations can model potential outcomes based on different dosing strategies or patient demographics, allowing researchers to refine their study designs before implementation. In summary, Phase 1 clinical trials are foundational to understanding new therapeutic agents’ safety and efficacy profiles in humans. As methodologies continue to advance through innovative designs and technologies, researchers are better equipped to navigate this complex landscape while prioritizing participant safety and data integrity.