The advent of virtual platforms has initiated a significant transformation in the landscape of clinical trials. Historically, clinical trials have operated as geographically constrained, in-person endeavors, requiring participants to visit physical sites for assessments, procedures, and data collection. This traditional model, though foundational to medical advancement, has presented numerous challenges, including recruitment difficulties, participant retention issues, and inherent logistical complexities. The COVID-19 pandemic acted as a powerful catalyst, accelerating the adoption of digitally enabled solutions and highlighting the potential for virtual platforms to overcome these limitations.
The traditional clinical trial is akin to a meticulously crafted, but geographically isolated, observatory. Researchers meticulously collect data from participants who make the pilgrimage to this specific location. While this focused approach has yielded invaluable insights, its reach is limited by distance and participant availability. Virtual platforms, in contrast, create a distributed network, a constellation of observational points that can be accessed from nearly anywhere. This fundamental shift redefines the very fabric of how clinical research is conducted, moving from a localized event to a decentralized, accessible process.
The Limitations of the Traditional Model
The established methodology of clinical trials, while effective, has long grappled with inherent constraints. These limitations have historically acted as speed bumps, slowing the pace of medical innovation and impacting the broader accessibility of research. Understanding these past challenges is crucial to appreciating the transformative impact of virtual platforms.
Patient Recruitment and Accessibility Barriers
Recruitment is often described as the lifeblood of any clinical trial. In the traditional model, this process is heavily reliant on geographical proximity. Patients must live within a reasonable commuting distance of a trial site to participate. This creates a significant barrier, particularly for individuals in rural areas, those with limited mobility, or those residing in regions underserved by research centers. The pool of potential participants is thus artificially constrained, often leading to extended recruitment timelines and, in some cases, the inability to enroll sufficient numbers to achieve statistical significance. This can be visualized as trying to fill a reservoir with a narrow pipe, severely limiting the volume and speed of water flow.
Participant Retention and Burden
The commitment required from participants in traditional trials can be substantial. Frequent site visits, often involving time off work, childcare arrangements, and travel expenses, place a significant burden on individuals. This strain can lead to decreased adherence to study protocols and, more critically, to participant attrition. When participants drop out, it undermines the integrity of the trial data, potentially leading to biased results or the need for additional recruitment efforts. The patient experience in a traditional trial can feel like a marathon with frequent, compulsory check-ins at distant aid stations, which, while necessary, can prove exhausting.
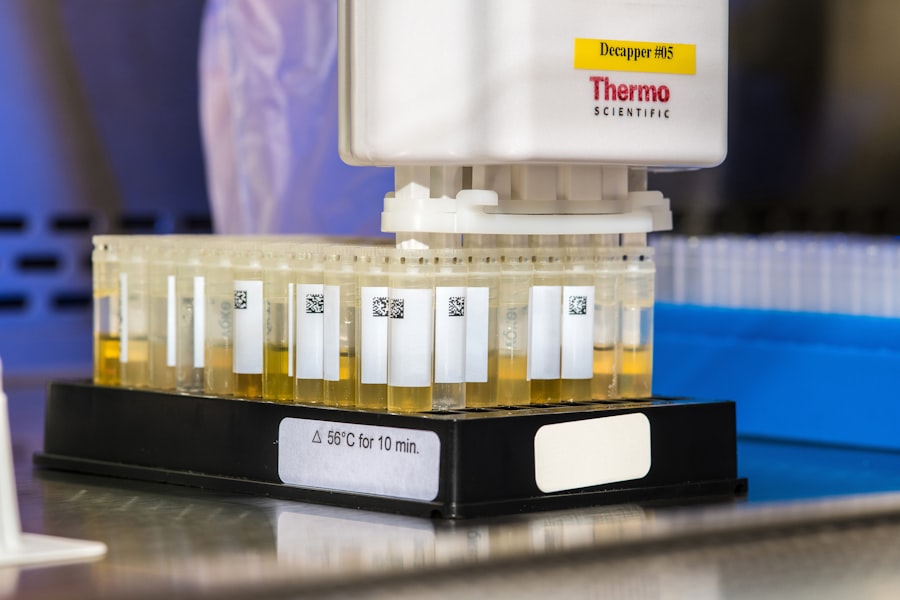
Logistical Complexities and Costs
Managing a network of physical trial sites incurs considerable logistical overhead. Site initiation, monitoring, equipment maintenance, and sample management all contribute to the complexity and cost of trials. Furthermore, the need for specialized personnel at each site adds to the expense. This intricate web of operations can be resource-intensive, diverting funds and attention that could otherwise be focused on scientific advancement. The traditional approach often resembles managing a fleet of individual ships, each requiring its own captain, crew, and maintenance schedule, making coordination across the fleet a monumental task.
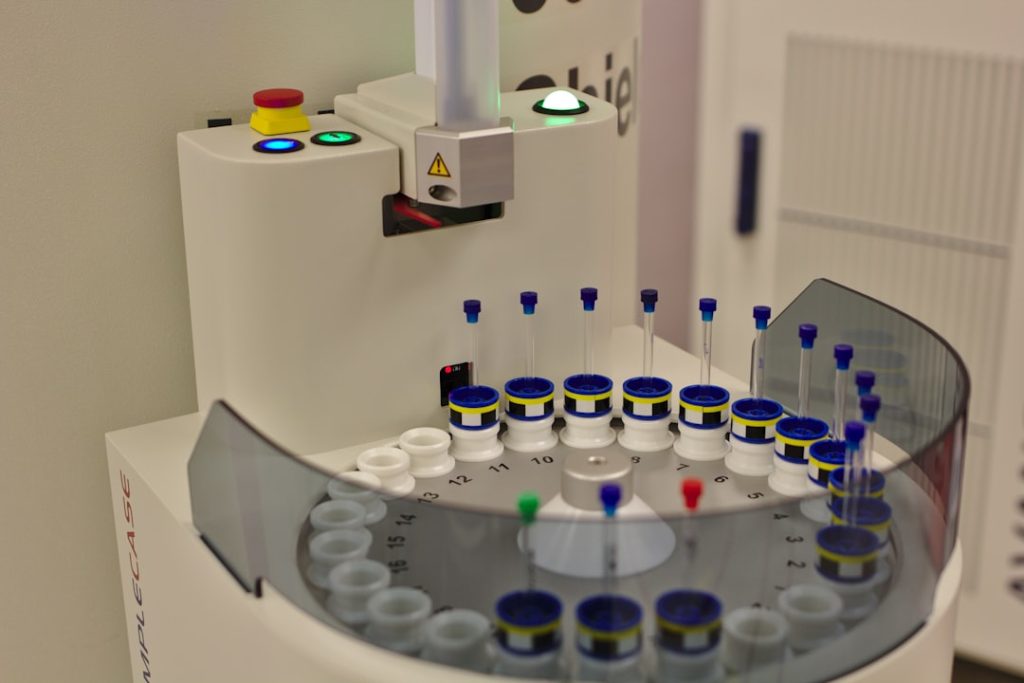
Core Components of Virtual Clinical Trials
Virtual platforms are not a singular technology but rather a mosaic of interconnected digital tools and processes designed to facilitate remote trial operations. These components work in concert to extend the reach and efficiency of clinical research, allowing for a more fluid and participant-centric approach.
Decentralized Data Collection and Monitoring
One of the cornerstones of virtual trials is the ability to collect data remotely. This is achieved through a variety of technological means, allowing for the continuous and unobtrusive capture of information. Instead of a single, central vault for information, virtual platforms create a distributed ledger, accessible and continuously updated from various points.
Wearable Devices and Biosensors
Wearable devices, such as smartwatches and fitness trackers, coupled with more specialized biosensors, are instrumental in passive data collection. These devices can continuously monitor vital signs like heart rate, activity levels, sleep patterns, and even specific physiological markers relevant to a particular condition. This constant stream of real-world data provides a richer and more ecologically valid picture of a participant’s health status than intermittent snapshots taken during site visits. Think of these as an army of tiny data scouts, constantly reporting back from the field.
Electronic Health Records (EHRs) Integration
Seamless integration with Electronic Health Records (EHRs) allows for the automated and secure collection of relevant patient medical history and treatment data. This eliminates the need for manual data entry and reduces the risk of transcription errors, significantly improving data accuracy and efficiency. This integration acts as a direct pipeline, allowing essential information to flow unimpeded into the research database.
Remote Patient Reported Outcomes (PROs)
Patient Reported Outcomes (PROs) are crucial for capturing subjective experiences, such as pain levels, symptom severity, and quality of life. Virtual platforms facilitate this through electronic questionnaires that participants can complete at their convenience from any internet-connected device. This ensures that the patient’s voice, a critical element in assessing treatment efficacy and tolerability, is consistently heard. These digital surveys are like direct feedback channels, allowing the research team to tap directly into the participant’s lived experience.
Telemedicine and Remote Consultations
Telemedicine plays a pivotal role in maintaining the human connection and oversight essential for clinical trials. It bridges the geographical divide, allowing for real-time interactions between participants and the research team. This is the virtual equivalent of a mobile command center, allowing for remote guidance and assessment.
Virtual Visits and Assessments
Instead of traveling to a clinic, participants can engage in video consultations with investigators and study coordinators. These virtual visits can be used for initial screening, ongoing efficacy assessments, safety monitoring, and to address any participant concerns. This drastically reduces logistical burdens for participants and allows for more frequent check-ins if necessary.
Remote Informed Consent and Education
The informed consent process, a cornerstone of ethical research, can also be facilitated virtually. Prospective participants can receive detailed information about the trial, ask questions, and provide their consent through secure video conferencing and digital signature platforms. Similarly, educational materials and study instructions can be delivered and reviewed remotely. This ensures that participants are fully informed and comfortable with their involvement, regardless of their location.
Benefits and Advantages of Virtual Platforms

The adoption of virtual platforms offers a compelling suite of advantages that address the inherent limitations of traditional clinical trials. These benefits translate into more efficient, accessible, and participant-centric research. The advantages are like opening up new, unhindered channels for progress.
Enhanced Patient Recruitment and Diversity
By removing geographical barriers, virtual platforms significantly expand the potential participant pool. This allows for the recruitment of a more diverse patient population, reflecting the broader population affected by a disease. A wider net cast by these platforms translates into a more representative sample, leading to findings that are more generalizable and applicable to a wider array of individuals. This is akin to moving from a local community garden to a national agricultural showcase, able to draw from a much richer diversity of crops.
Reaching Underserved Populations
Virtual trials are particularly effective in reaching individuals in rural or remote areas, as well as those with limited mobility or access to transportation. This democratizes participation in clinical research, ensuring that individuals from all walks of life have the opportunity to contribute to medical advancement.
Broader Geographic Reach
The ability to recruit participants from across a country, or even internationally, allows researchers to enroll patients with specific rare conditions more rapidly than ever before. This is a significant boon for rare disease research, where finding enough participants in a single geographical area can be a protracted and often unsuccessful endeavor.
Improved Participant Experience and Retention
The reduced burden on participants directly impacts their willingness and ability to remain involved in a trial. By bringing the trial to the patient, virtual platforms foster a more positive and sustainable research experience. This leads to better adherence and ultimately, more robust trial data. A smoother journey for the participant means they are more likely to reach the intended destination.
Reduced Travel Burden and Time Commitment
Eliminating the need for frequent site visits dramatically reduces the time and financial costs associated with participation. This makes participating in clinical trials more feasible for a wider range of individuals, including those with demanding work schedules or family commitments.
Increased Privacy and Comfort
Completing some study activities from the comfort of one’s own home can enhance participant privacy and reduce anxiety associated with clinical settings. This can lead to more candid and accurate reporting of symptoms and experiences.
Streamlined Operations and Cost Efficiency
The operational advantages of virtual platforms translate into significant efficiencies and potential cost savings for trial sponsors. By reducing reliance on physical infrastructure and optimizing data management, resources can be reallocated to more critical research activities. These efficiencies are like trimming excess weight from an aircraft, allowing it to fly further and more smoothly.
Reduced Site Management Overhead
Decentralizing operations reduces the need for extensive site infrastructure, management, and monitoring personnel. This can lead to substantial savings in operational costs.
Accelerated Data Analysis and Timelines
The continuous and real-time collection of data through virtual platforms facilitates more rapid data analysis. This can lead to expedited clinical trial timelines, allowing potentially life-saving treatments to reach patients sooner.
Challenges and Considerations for Virtual Platforms
While the benefits of virtual platforms are substantial, their implementation is not without its own set of hurdles. Addressing these challenges is crucial for the widespread and successful integration of these innovative approaches into clinical research. Navigating these challenges requires careful planning and execution, much like charting a course through sometimes unpredictable waters.
Data Security and Privacy Concerns
The collection and transmission of sensitive patient data in a digital environment raise paramount concerns regarding security and privacy. Robust safeguards must be in place to protect against unauthorized access, data breaches, and potential misuse. Ensuring the integrity and confidentiality of this information is non-negotiable.
Robust Cybersecurity Measures
Implementing state-of-the-art encryption, multi-factor authentication, and regular security audits are essential to protect data throughout its lifecycle. The digital infrastructure must be as fortified as a national treasury.
Compliance with Data Protection Regulations
Strict adherence to regulations such as HIPAA (in the US) and GDPR (in Europe) is mandatory. These regulations dictate how patient data can be collected, stored, and used, ensuring participant rights are upheld.
Digital Divide and Technological Literacy
Not all individuals have equal access to reliable internet connectivity or possess the necessary technological literacy to navigate virtual platforms. This digital divide could inadvertently exclude certain segments of the population from participating in trials. Bridging this gap is a critical step towards equitable access.
Ensuring Accessibility for All
Strategies such as providing participants with necessary devices, offering technical support, and developing user-friendly interfaces are crucial to overcome these disparities. This might involve a digital outreach program, akin to public library initiatives.
Training and Support for Participants
Comprehensive training sessions and easily accessible technical support are vital to ensure participants can comfortably and confidently engage with the virtual platform. This empowers individuals to be active participants, not passive observers.
Regulatory Acceptance and Standardization
The regulatory landscape for virtual and decentralized clinical trials is still evolving. While regulatory bodies are increasingly embracing these approaches, there can be varying requirements and a need for greater standardization to ensure consistency and facilitate global adoption. Gaining regulatory approval can sometimes feel like navigating a complex maze, and for new methodologies, the paths are still being mapped out.
Harmonizing Regulatory Frameworks
Continued collaboration between regulatory agencies, industry, and research institutions is necessary to develop clear, harmonized guidelines for virtual trial operations. This fosters trust and predictability.
Validation of Digital Tools
Ensuring the validity and reliability of digital endpoints and data capture methods is critical for regulatory acceptance. Thorough validation processes are akin to rigorous scientific peer review for new technologies.
The Future of Clinical Trials: A Hybrid Landscape
| Metric | Description | Typical Value / Range | Importance |
|---|---|---|---|
| Patient Enrollment Rate | Number of patients enrolled per month | 50 – 200 patients/month | High – impacts trial timelines |
| Patient Retention Rate | Percentage of patients completing the trial | 85% – 95% | High – ensures data completeness |
| Data Collection Frequency | Number of data points collected per patient per day | 1 – 5 data points/day | Medium – affects data granularity |
| Protocol Deviation Rate | Percentage of deviations from trial protocol | 1% – 5% | Medium – impacts data quality |
| Time to Database Lock | Duration from last patient visit to database lock | 2 – 4 weeks | High – affects study closeout speed |
| Cost per Patient | Average cost to enroll and manage one patient | 1,000 – 5,000 | High – impacts overall trial budget |
| Adverse Event Reporting Time | Time taken to report adverse events | Within 24 hours | Critical – ensures patient safety |
| Platform Uptime | Percentage of time the platform is operational | 99.5% – 99.9% | High – ensures continuous data capture |
| Patient Satisfaction Score | Average rating from patient feedback surveys | 4.0 – 4.8 (out of 5) | Medium – affects patient engagement |
The future of clinical trials is not likely to be entirely virtual or entirely traditional. Instead, the most effective model will likely be a hybrid approach, leveraging the strengths of both in-person and virtual methodologies. This blended approach offers a balanced solution, maximizing efficiency and accessibility while retaining the essential elements of direct patient-physician interaction. The future is a well-orchestrated symphony, where different instruments play their distinct parts to create a harmonious whole.
Integrating Virtual and Traditional Elements
Hybrid trials integrate virtual components, such as remote data collection and telemedicine, with essential in-person visits for specific assessments or procedures. This allows for the flexibility of virtual engagement while maintaining crucial physical interactions. This is akin to a well-equipped laboratory that also includes field research capabilities.
Strategic Design of Hybrid Trials
Careful consideration must be given to which trial activities are best suited for virtual execution and which require in-person engagement, based on the specific study protocol and participant needs. This requires strategic design, ensuring the right tool is used for the right job.
Leveraging Technology for Enhanced In-Person Visits
Even for in-person visits, technology can enhance the experience. For example, pre-visit questionnaires completed virtually can streamline the on-site appointment, allowing more time for physician-patient interaction during the visit itself.
Impact on Drug Development and Patient Care
The widespread adoption of virtual platforms has the potential to accelerate drug development timelines, bring innovative treatments to market faster, and ultimately improve patient outcomes and access to cutting-edge medical care. This transformation has a ripple effect, positively impacting both the speed of discovery and the quality of life for patients. The acceleration in drug development can be seen as a faster courier service for life-saving medicines.
Faster Access to Novel Therapies
By streamlining recruitment and data collection, virtual trials can significantly shorten the time it takes to bring new drugs and therapies from discovery to market, offering hope to patients facing unmet medical needs.
Empowering Patients in Their Healthcare Journey
Virtual platforms empower patients to take a more active role in their healthcare and research participation. This shift towards patient empowerment fosters greater engagement and a more collaborative approach to medical advancement.
The revolution in clinical trials brought about by virtual platforms represents a significant leap forward in how medical research is conducted. By embracing digital innovation, the field is moving towards a more accessible, efficient, and patient-centric future, promising to accelerate the development of life-changing therapies and enhance global health outcomes.