Investigational Device Exemptions (IDE) are a critical component of the medical device regulatory framework in the United States, allowing for the clinical investigation of devices that have not yet received full approval from the Food and Drug Administration (FDA). The IDE process is designed to facilitate the development and testing of innovative medical technologies while ensuring patient safety and data integrity. By granting exemptions, the FDA enables manufacturers to gather essential clinical data that can demonstrate a device’s safety and effectiveness, ultimately paving the way for market approval.
This regulatory pathway is particularly significant in a rapidly evolving healthcare landscape, where the demand for novel solutions to complex medical challenges is ever-increasing. IDE medical devices encompass a wide range of technologies, from cutting-edge surgical instruments to advanced diagnostic tools. These devices are often at the forefront of medical innovation, addressing unmet clinical needs and improving patient care.
The IDE process not only allows for the exploration of new therapeutic avenues but also encourages collaboration between researchers, clinicians, and manufacturers. As a result, IDE medical devices play a pivotal role in advancing healthcare by fostering an environment where experimentation and innovation can thrive, ultimately leading to improved treatment options for patients.
Key Takeaways
- IDE medical devices are innovative tools designed to enhance diagnostic and therapeutic processes in healthcare.
- They significantly improve patient outcomes by enabling more precise and personalized treatments.
- Compared to traditional devices, IDE medical devices offer advantages such as increased accuracy, efficiency, and real-time data monitoring.
- Challenges include regulatory hurdles, ethical concerns, and technical limitations that must be addressed for widespread adoption.
- Future advancements and innovations in IDE medical devices hold promise for transforming healthcare delivery and patient care.
The Impact of IDE Medical Devices on Healthcare
The introduction of IDE medical devices has had a profound impact on healthcare delivery and patient outcomes. By enabling the clinical evaluation of new technologies, IDEs have accelerated the pace at which innovative solutions can be brought to market. This rapid development cycle is particularly crucial in fields such as cardiology, oncology, and neurology, where timely access to new treatments can significantly alter disease trajectories.
For instance, the use of IDEs has facilitated the introduction of novel stents and drug-eluting devices that have transformed the management of coronary artery disease, leading to better patient prognoses and reduced mortality rates. Moreover, IDE medical devices have contributed to a more personalized approach to medicine. As these devices undergo clinical trials, they often incorporate advanced data analytics and artificial intelligence to tailor treatments to individual patient profiles.
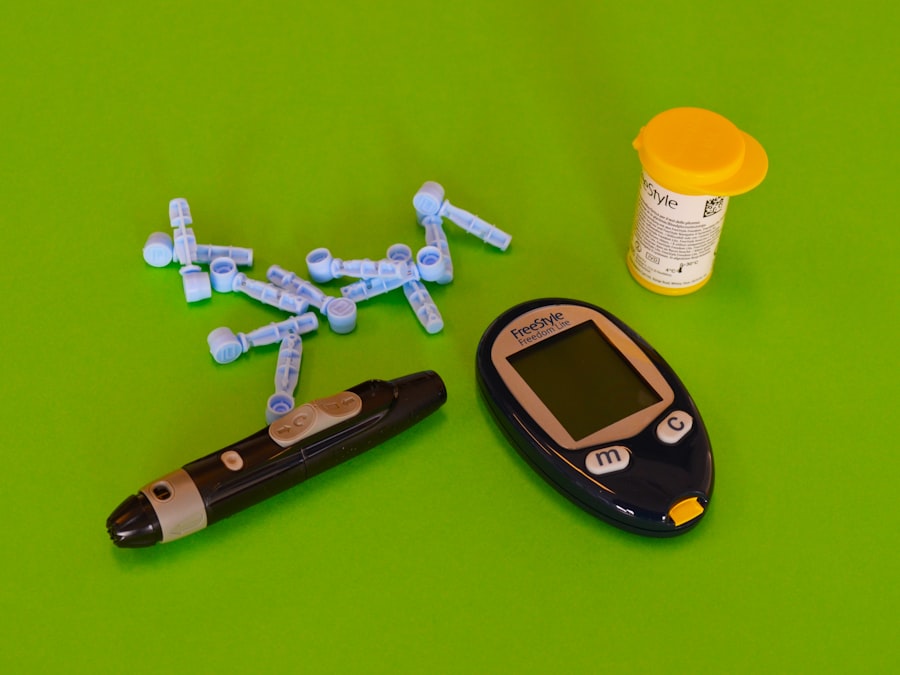
This shift towards precision medicine is exemplified by IDE studies that explore the efficacy of wearable devices in monitoring chronic conditions such as diabetes or hypertension. By collecting real-time data on patient health metrics, these devices empower healthcare providers to make informed decisions and adjust treatment plans proactively, ultimately enhancing patient engagement and adherence.
Advantages of IDE Medical Devices over Traditional Medical Devices

One of the primary advantages of IDE medical devices is their ability to undergo rigorous clinical testing before receiving full market approval. This process allows for comprehensive evaluation of safety and efficacy in diverse patient populations, which is often not feasible with traditional medical devices that may rely on pre-market notifications or 510(k) submissions. For example, an IDE study may involve multiple clinical sites and a large cohort of participants, providing robust data that can inform best practices and clinical guidelines.
In contrast, traditional devices may lack such extensive validation, potentially leading to variability in performance across different settings. Additionally, IDE medical devices often benefit from a more flexible regulatory framework that encourages innovation. The FDA recognizes the need for rapid advancements in technology and has established mechanisms such as the Breakthrough Devices Program to expedite the development of devices that offer significant benefits over existing options.
This flexibility allows manufacturers to explore novel designs and functionalities that may not fit within the constraints of traditional regulatory pathways. As a result, IDE medical devices can introduce groundbreaking features—such as minimally invasive techniques or integrated digital health solutions—that enhance patient care and improve overall healthcare efficiency.
The Role of IDE Medical Devices in Improving Patient Outcomes
The role of IDE medical devices in improving patient outcomes cannot be overstated. By facilitating the development of innovative technologies that address specific clinical needs, these devices have the potential to transform treatment paradigms across various medical specialties. For instance, in orthopedics, IDE studies have led to the introduction of advanced implants that promote faster healing and improved functionality for patients undergoing joint replacement surgeries.
These innovations not only enhance surgical outcomes but also reduce recovery times, allowing patients to return to their daily activities more quickly. Furthermore, IDE medical devices often incorporate feedback from both clinicians and patients during the development process. This collaborative approach ensures that the resulting technologies are user-friendly and aligned with patient preferences.
For example, in the realm of diabetes management, IDE studies have explored the use of continuous glucose monitoring systems that provide real-time data to patients and their healthcare teams. By empowering patients with actionable insights into their health, these devices facilitate better self-management and ultimately lead to improved glycemic control and reduced complications.
Challenges and Limitations of IDE Medical Devices
| Metric | Description | Typical Values | Unit |
|---|---|---|---|
| Device Sensitivity | Ability of the device to correctly identify positive cases | 85 – 98 | % |
| Device Specificity | Ability of the device to correctly identify negative cases | 90 – 99 | % |
| Power Consumption | Average electrical power used during operation | 0.5 – 5 | Watts |
| Operating Temperature Range | Temperature range within which the device operates reliably | 10 – 40 | °C |
| Battery Life | Duration the device can operate on a full charge | 8 – 24 | Hours |
| Response Time | Time taken to provide a measurement or output | 1 – 10 | Seconds |
| Weight | Physical weight of the device | 100 – 500 | Grams |
| Dimensions | Physical size of the device (L x W x H) | 10 x 5 x 3 | cm |
| Regulatory Approval | Certification status for clinical use | FDA IDE, CE Mark | N/A |
Despite their numerous advantages, IDE medical devices also face several challenges and limitations that can hinder their development and implementation. One significant challenge is the complexity of conducting clinical trials for these devices. The process often requires substantial financial investment and resources, which can be a barrier for smaller companies or startups looking to bring innovative solutions to market.
Additionally, recruiting a sufficient number of participants for clinical trials can be difficult, particularly for devices targeting rare conditions or specific patient populations. Another limitation is the potential for variability in trial outcomes due to differences in study design or patient demographics. While IDE studies aim to provide comprehensive data on device performance, factors such as site variability or patient adherence can influence results.
This variability may complicate the interpretation of findings and raise questions about generalizability across broader populations. Furthermore, as technology evolves rapidly, there is a risk that findings from an IDE study may become outdated by the time a device receives market approval, necessitating ongoing research to ensure continued relevance.
Future Prospects and Innovations in IDE Medical Devices
The future prospects for IDE medical devices are promising, with ongoing advancements in technology poised to reshape the landscape of healthcare delivery. One area ripe for innovation is the integration of artificial intelligence (AI) and machine learning into device design and functionality. These technologies can enhance diagnostic accuracy, optimize treatment protocols, and improve patient monitoring capabilities.
For instance, AI algorithms can analyze vast amounts of data generated by wearable devices to identify patterns that may indicate disease progression or treatment response, enabling more proactive interventions. Moreover, as telemedicine continues to gain traction, there is an opportunity for IDE medical devices to incorporate remote monitoring capabilities that facilitate virtual care models. Devices designed for home use can empower patients to manage their health conditions independently while maintaining connectivity with their healthcare providers.
This shift towards decentralized care not only enhances patient convenience but also reduces healthcare costs by minimizing hospital visits and readmissions.
Regulatory and Ethical Considerations in the Use of IDE Medical Devices
The regulatory landscape surrounding IDE medical devices is complex and requires careful navigation to ensure compliance with established guidelines while fostering innovation. The FDA plays a crucial role in overseeing the IDE process, ensuring that clinical trials are conducted ethically and that participant safety is prioritized. Manufacturers must adhere to stringent protocols regarding informed consent, data collection, and reporting adverse events throughout the trial period.
Ethical considerations also extend beyond regulatory compliance; they encompass issues related to equity in access to innovative treatments. As IDE medical devices are developed and tested primarily within specific populations or geographic regions, there is a risk that certain groups may be underrepresented in clinical trials. This lack of diversity can lead to disparities in treatment outcomes when these devices are eventually introduced into broader patient populations.
Addressing these ethical concerns requires a commitment from manufacturers and researchers to engage diverse communities in the development process and ensure equitable access to emerging technologies.
The Future of Healthcare with IDE Medical Devices
The trajectory of healthcare is increasingly intertwined with the advancements brought forth by IDE medical devices. As these innovative technologies continue to evolve through rigorous clinical testing and regulatory oversight, they hold the potential to revolutionize patient care across various domains. The integration of cutting-edge features such as AI-driven analytics and remote monitoring capabilities will further enhance their impact on healthcare delivery.
As we look ahead, it is essential for stakeholders—including manufacturers, clinicians, regulators, and patients—to collaborate closely in navigating the challenges associated with IDE medical devices. By fostering an environment that prioritizes innovation while upholding ethical standards and regulatory compliance, we can ensure that these transformative technologies are harnessed effectively for the benefit of all patients. The future of healthcare is bright with the promise of IDE medical devices leading the way toward improved outcomes and enhanced quality of life for individuals around the globe.




